Abstract
Medication-related osteonecrosis of the jaw (MRONJ) is a rare but major complication related to the use of anti-resorptive and anti-angiogenic drugs. The risk of MRONJ is well established in the adult population, however, is still unknown in the paediatric population with few reports that investigate the risk of MRONJ in paediatric patients. Dentists play a significant role in the management of paediatric patients with the risk of MRONJ from identifying the risk, maintaining oral health to collaborating with other specialities to provide high quality care. This case report provides detailed insight into the management of a paediatric patient with prolonged exposure to antiresorptive drug undergoing dental extraction.
Keywords:Medication-related Osteonecrosis of The Jaw (MRONJ); Bisphosphonates; Antiresorptive; Antiangiogenic
Introduction
MRONJ is defined as exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for more than eight weeks in patients with a history of treatment with antiresorptive or antiangiogenic drugs, where there has been no history of radiation therapy to the jaw or no obvious metastatic disease to the jaws [1]. The exact pathophysiology of the disease is not yet fully known whilst possible factors include inhibition of bone turnover, infection or inflammation, inhibition of angiogenesis and immune dysfunction. Risk factors include the underlying medical condition of the patient, cumulative drug dose, concurrent medication specifically systemic glucocorticoids, dentoalveolar surgery and mucosal trauma.
The risk of MRONJ in patients being treated with anti-resorptive drugs for osteoporosis or other non-malignant diseases of bone (0.01-0.1% incidence) is lower than patients being treated for cancer (1% incidence). The reported incidence for MRONJ for patients treated for osteoporosis with antiresorptive drugs is <0.05% [2]. The evidence for MRONJ in paediatric patients is insufficient with low presence of MRONJ in the child and youth population treated with antiresorptive drugs. Bisphosphonates and other antiresorptive/antiangiogenic drugs used by paediatric patients are on the increase and are used for conditions including osteogenesis imperfecta, idiopathic juvenile osteoporosis, rheumatologic disorders, Crohn’s disease, malignant hypercalcaemia and other conditions [3]. Currently there are few reports in children and adolescents who are treated with antiresorptive/antiangiogenic agents undergoing invasive dental treatment. The aim of this case report is to provide information on the management of patients who are at risk of developing MRONJ in such patients.
Case Report
A 10-year-old female was referred in June 2022 to tertiary care in hospital to the specialists in Paediatric Dentistry by the Community Dental Service for treatment of unrestorable carious upper right first permanent molar tooth and dental anxiety. Treatment modalities were discussed of local anaesthetic with or without inhalation sedation and treatment under general anesthetic. Given the patient’s anxiety and unsuccessful attempt with inhalation sedation, patient and parent opted for dental treatment under general anesthetic. Medically, she was diagnosed with Takayasu’s arteritis at the age of 7 and started on Prednisolone, 50mg daily. A diagnosis 3 years later of osteoporosis secondary to chronic glucocorticoid treatment and her chronic inflammatory condition of Takayasu’s arteritis. The dose for Prednisolone was weaned overtime with continued doses of 3mg daily. During her initial treatment, she required prolonged admission and intermittent doses of 15mg/kg IV Methylprednisolone. She also had Methotrexate 20mg subcutaneously weekly and Adalimumab 40mg subcutaneously every 2 weeks. When Adalimumab was stopped, she started on subcutaneous Tocilizumab 162mg 2 weekly. She was on Pamidronate disodium 1 mg/kg daily for 3 days every 3 months for 15 months.
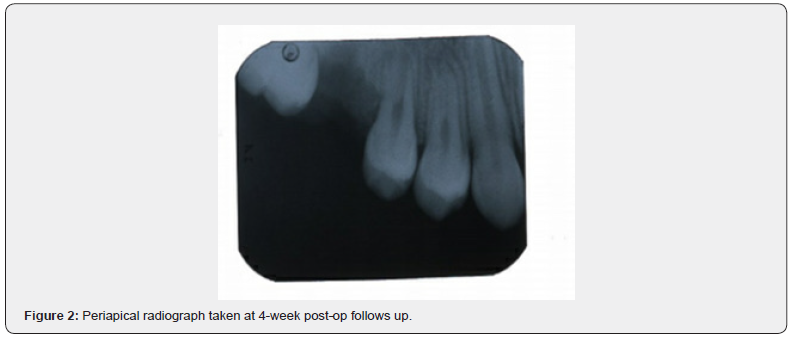
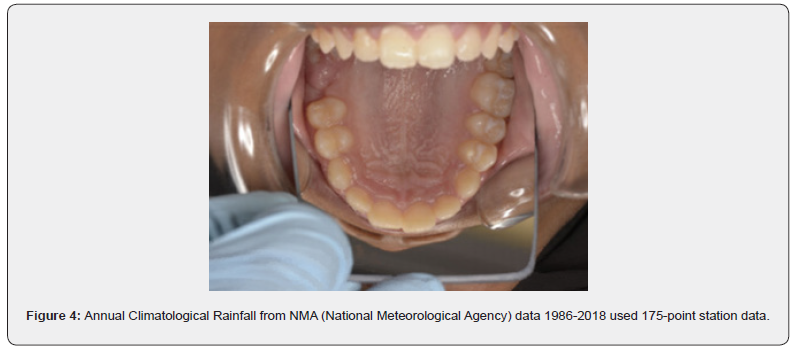
An up-to-date medical history and correspondence from other health professionals involved in her care including paediatrician, rheumatology, endocrinology and pharmacist was obtained regarding complete and comprehensive information about the patient’s medical condition and drug regimens. A consultant led general anaesthetic pre-assessment was also carried out. She presented with unreasonable oral hygiene, multiple carious decayed teeth and unrestorable upper left first permanent molar (Figure 1). A nasotracheal intubation was used in the general anaesthetic. Treatment involved scale and polish, multiple composite restorations of the lower left first permanent molars and lower left second permanent molar. The upper right first permanent molar was extracted a traumatically with the roots and apices intact (Figure 2 & Figure 3). A post-operative review took place a week, 2, 4, 6 and at 8 weeks. Patient did not complain of any pain or symptoms. Intra-orally, the extraction site healed with no concerns with no significant difference in time of healing. Oral hygiene was unreasonable at 4 weeks with generalised plaque build-up noted and marginal gingivitis. Oral hygiene and diet advice were reinforced at each appointment with personalised preventive advice. Patient did not develop MRONJ and was discharged back to their General Dental Practitioner for routine dental care and close monitoring.
Discussion
There are some factors that may increase an individual’s risk of MRONJ and so influence their dental management. The risk can be higher if undergoing dentoalveolar surgery or any procedure that impacts bone although MRONJ can occur spontaneously. The duration of the drug is thought to increase the risk and other concurrent medication especially chronic systemic glucocorticoids and combination of other bisphosphonates and/or antiangiogenic/antiresorptive drugs. Current evidence shows no evidence of MRONJ in the child and youth population although data collection is weak with details of therapy not clear [4]. Further studies are needed to clarify the risk of MRONJ in the paediatric population and the long-term cumulative effects of anti-resorptive and angio-genic. A case report on a nine-year-old female patient presented with a vertebral aneurysmal bone cyst, who received dental extractions following denosumab therapy. The report highlighted the possible impact of dental treatment on children on antiresorptive medication and the need for reporting cases [5]. Manley et al, reported on an adolescent at the age of 23 who developed MRONJ spontaneously who received long-term antiresorptive medication since the age of 166.
Further research is required to establish a definitive consensus in the management of children on these drug therapies. A study showed no definitive consistency among paediatric dentists in managing paediatric patients taking bisphosphonates [6,7]. Prevention is crucial in reducing the risk for MRONJ. Before commencing antiresorptive or antiangiogenic drug therapy, patients should be aimed to be as dentally fit as feasible. Continued personalised preventive advice is important to always optimise oral health. This case report highlighted that despite regular appointments with the dentist, oral hygiene and diet must be monitored and advice reinforced regularly. Patients and their parents/guardian should be aware of the medication they are taking and their risk of developing MRONJ. Children who are prescribed antiresorptive/angiogenic drugs with a risk of MRONJ are likely to be managed by specialists in paediatric dentistry depending on their treatment required.
Conclusion
Paediatric patients on antiresorptive or anti-angiogenic drug therapy must be monitored closely and oral health promotion is fundamental. All dentists must be aware of the risk MRONJ and appropriate management of these patients on such treatment. Further studies are required to ascertain the risk of MRONJ in paediatric patients as well as reporting cases on the management of these patients and their transition to adolescents.
References
- (2024) Scottish Dental Clinical Effectiveness Programme. Oral Health Management of Patients at Risk of Medication-related Osteonecrosis of the Jaw. Dental Clinical Guidance.
- Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, et al. (2022) American Association of Oral and Maxillofacial Surgeons' Position Paper on Medication-Related Osteonecrosis of the Jaws-2022 Update. Journal of Oral and Maxillofacial Surgery 80(5): 920-943.
- Baroncelli G, Bertelloni S (2014) The use of bisphosphonates in paediatrics. Horm Res Paediatr 82(5): 290-302.
- Rosales HD, Garcia Guevara H, Requejo S, Jensen MD, Acero J, et al. (2023) Medication-Related Osteonecrosis of the Jaws (MRONJ) in Children and Young Patients-A Systematic Review. J Clin Med 12(4): 1416.
- Innes-Taylor D, Adams V (2024) Medication-related osteonecrosis of the jaw in a paediatric patient taking denosumab: a case report. Br Dent J 236(6): 453-456.
- Manley BJ, Neal TW, Indrakanti S, Schlieve T (2023) Spontaneous medication-related osteonecrosis of the jaws in a 23-year-old. Oral and Maxillofacial Surgery Cases 9(1): 100289.
- Lau, Jeremy, Ng Lei, Siddiqi Allauddin, Zafar Sobia (2019) Paediatric Dentists Treating Children on Bisphosphonates: A Cross-Sectional Questionnaire-Based Study. Pediatric dentistry 41(4): 285-292.






























