Abstract
This study aims to evaluate the influence of dental preparations and two types of ceramic on the fracture resistance and marginal adaptation of teeth restored with laminate veneers. 56 central incisors were divided into 7 groups, according to the type of dental preparation: window, straight edge, overlap; and the type of ceramic: feldspathic and lithium disilicate. After cementation of veneers with resin luting cement, replicas in epoxy resin were evaluated regarding marginal gap in scanning electron microscopy (SEM). The results were statistically analyzed by ANOVA and Chi square test, with a significance level of 5%. The restored teeth resistance was significantly influenced by the type of preparation (p = 0.03) and ceramic (p = 0.011). The best performance was the lithium disilicate ceramic, associated with the straight edges and overlap preparations. Within the feldspathic ceramic group, the best strength was associated with the window preparation type. About the marginal adaptation analysis, groups with straight edge and overlap preparations associated with lithium disilicate ceramic showed no marginal gaps. The group with window preparation with lithium disilicate ceramic and group straight edge with feldspathic ceramic showed 75% of gap presence. It is concluded that, for feldspathic ceramic, the window preparation showed better fracture resistance. For lithium disilicate ceramic, the type of preparation did not influence the fracture resistance. When the incisal edge is involved, laminate veneers built with lithium disilicate ceramic associated with the straight edge or overlap preparations showed no gap formation and had the best fracture resistance.
Keywords:Ceramics; Dental veneers; Aesthetics
Abbreviations:SEM: Scanning electron microscopy; N: Newtons; SD: Standard deviation
Introduction
In current Dentistry, there is a constant search to develop restorative materials with good physical, mechanical, biological and aesthetic properties that can restore the dental element. With this continuous advancement, the dentist has different modalities of restorative treatment at his disposal, which include composite resins and ceramics [1]. This fact, combined with the increasing demand from patients for more durable and aesthetic restorations in the anterior teeth, has resulted in a considerable increasing in the use of ceramic veneers [2]. Veneers were first described in 1937 by Charles Pincus and used in the movies industry as a method to optimize the dental aesthetic and the smile of actors [3]. Therefore, veneers have been used frequently and are, basically, indicated as a conservative restorative means for aesthetically disadvantaged anterior teeth [4]. Ceramic laminate veneers represent an aesthetic restorative option that combines minimal dental wear and provides significant and lasting aesthetic improvement [5,6]. The clinical success of ceramic laminate veneers is mentioned in several works in the literature, where observation periods for some veneers exceed 20 years of follow-up [3]. In cases where ceramic veneers fail, the most often cited failures are fractures, microleakage and decementation [7,8]. Many factors can influence the long-term success of this type of restoration, such as: tooth substrate, ceramic thickness, type of luting agent, adhesive system used, marginal adaptation, periodontal response, functional and parafunctional activities performed by the patient, the type of ceramic and tooth preparation [6,9,10].
Three types of dental preparation for ceramic veneers have been most frequently described. The window type preparation limited to the wear of the buccal surface of the tooth, leaving the enamel incisal edge intact [11]; the straight edge type preparation includes the incisal edge, reducing it with a straight end; the overlap type preparation reduces and overlaps the incisal edge, presenting a lingual chamfer [2]. For some authors, incisal coverage improves the mechanical resistance of the laminate veneers [2] and contributes to a better distribution of forces, reducing fractures [12], despite greater reduction of dental structure [10]. Zarone et al. [9] indicate that the extension of the incisal margin allows a distribution of the occlusal load, reducing the stress concentration of the veneer, as well as increasing the adhesive surface. Clinical studies demonstrate better results for ceramic veneers prepared with incisal coverage, or do not show differences when comparing different types of preparations. Thus, there is no consensus on which preparation is ideal for laminate veneer restorations [11].
The type of ceramic material chosen also plays an important role, and it is necessary to evaluate how laminate veneers of different materials respond in terms of fracture resistance and marginal sealing. There are mainly two types of ceramic systems for veneers, feldspathic ceramics and reinforced glass ceramics, such as leucite and lithium disilicate, which enable the internal surface conditioning with hydrofluoric acid and the application of silane, providing bonding capacity to the surface and significantly increasing the bond strength of luting cement to ceramic [6,13]. Therefore, it is not clear in the literature how the dental preparation associated with different types of ceramic materials can influence the fracture resistance and marginal adaptation of veneers. As a matter of fact, ceramic laminate veneers are restorations often performed by dentists and can be influenced by the different types of dental preparation [14], and by the different types of ceramic with their differences in terms of mechanical behavior [15]. Thus, this work aims to evaluate the influence of dental preparation (window, straight edge and enveloped edge) and different types of ceramic (feldspathic and lithium disilicate) on the fracture resistance and marginal adaptation of teeth restored with laminate veneers.
Materials and Methods
To carry out the analysis of fracture resistance and marginal
adaptation of teeth restored with ceramic veneers with different
types of preparation and ceramic, healthy upper central incisors
were selected, extracted for therapeutic reasons (approval by
the UFRGS Research Ethics Committee). The teeth had no cracks,
fractures, caries lesions or previous restorations, and were kept
in distilled water until the beginning of the study. Fifty-six healthy
human central incisors were used, divided into seven groups
(n=08), according to sample calculation:
i. Group 1 (control): sound teeth.
ii. Group 2 (WF): teeth with window-type preparation +
feldspathic ceramic veneers.
iii. Group 3 (WLD): teeth with window-type preparation +
lithium disilicate ceramic veneers.
iv. Group 4 (SEF): teeth with straight edge-type preparation
+ feldspathic ceramic veneers.
v. Group 5 (SELD): teeth with straight edge-type
preparation + lithium disilicate ceramic veneers.
vi. Group 6 (OF): teeth with overlap-type preparation +
feldspathic ceramic veneers.
vii. Group 7 (OLD): teeth with overlap-type preparation +
lithium disilicate ceramic veneers.
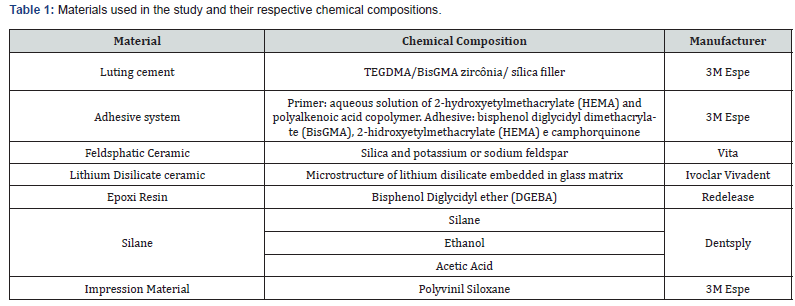
Prior to the dental preparations, the teeth were disinfected in 0.5% chloramine for 7 days. Each tooth had its root included in cylinders with self-polymerizing acrylic resin (Jet) and fixed in its long axis 2 mm below the cementoenamel junction. Afterwards, the teeth had impression taking with polyvinyl siloxane (Express XT – 3M Espe), to obtain a preparation guide (profile) for guidance, control and standardization of wear thickness during preparations. The main materials used in this study are described in Table 1.
Teeth Preparation
Teeth preparations for groups 2-7 were carried out with diamond burs (KG Sorensen) under constant water-cooling at high speed (Kavo). These preparations were started in the cervical region with a 1014 diamond bur, 1 mm below the cementoenamel junction, this bur was positioned 45 degrees in relation to the long axis of the tooth. A wear of 0.5 mm deep was made on the buccal surface (guide by the lateral guide), made with a diamond bur number 2135. A diamond bur number 4138 concluded the convexity of the buccal surface in the cervical, middle and incisal thirds. The buccal wear was 0.5 mm in all groups. Groups 4-7, had an incisal reduction of 2 mm [14], performed with the same diamond bur (4138). The dental preparations in groups 4 and 5 (straight edge), only had a reduction of the incisal edge, ending at an angulation of 90 degrees with the palatal surface. The dental preparations of groups 6 and 7 (overlap), presented, in addition to the incisal reduction of 2 mm, a chamfer on the palatal surface with a thickness of 1 mm. Each diamond bur prepared 5 teeth, being replaced by another of the same kind. All preparations were carried out by the same operator. To finish and smooth the preparations, fine-grained diamond burs (4138F - KG Sorensen) were used, followed by abrasive silicon points (Enhance - Dentsply).
Dental Impressions
After the preparations, impressions were taken from each tooth with polyvinyl siloxane (Express XT – 3M Espe, putty and light material), to obtain the gypsum dental cast (Durone IV - Dentsply) and subsequent production of the laminate veneers.
Luting Cement Procedures
Feldspathic ceramic as well as lithium disilicate were manufactured according to the manufacturer’s instructions, in a Dental laboratory with experience in the respective ceramic systems. The feldspathic ceramic (Vita) was built on a refractory cast, using a sintering process, while lithium disilicate ceramic (IPS e.max press, Ivoclar Vivadent) was injected (pressed). For the luting process, the veneers built with feldspathic ceramics were etched with 10% hydrofluoric acid (Condac 10% - FGM) for 60 seconds, while the veneers built with lithium disilicate were etched with the same acid for 20 seconds. All veneers were washed thoroughly with water to remove the acid and dried with air. Two coats of Silane were applied (Silane - Dentsply) for 1 minute, followed by air-drying, then the adhesive application was carried out (Adper Scothbond Multipurpose - 3M Espe) with microbrush, followed by lightcuring for 20 seconds, with an LED light curing device (Smart Light TM, Dentsply) with 600 mW/cm2, measured with a radiometer (Demetron).
Teeth were etched with 37% phosphoric acid (Condac 37 - FGM) starting with the enamel for 30 seconds and then on the dentin for 15 seconds, washed and dried with air. Afterwards, the adhesive system (Adper ScothBond Multipurpose, Primer and Adhesive), followed by lightcuring by 20 seconds with the same led mentioned above. Then, the luting cementation process of the veneers was carried out, using the resin cement RelyX Veneer (3M Espe, shade A1), inserted on veneers` surface. After lightcuring during 60 seconds around the veneers, finishing of the interface was carried out by scalpel blades, and polishing of the cementation line was performed with abrasive silicon points (Enhance, Dentsply). All specimens were kept under the distilled water for 24 hours, before testing [16].
Marginal Adaptation Analysis
After cementation, the specimens were thermocycled in 500 cycles of 5-55°C, remaining 30 seconds at each temperature. Then, an impression was taken with polyvinyl siloxane (putty and light) of each restored tooth with the aim of obtaining a replica of the veneer interfaces, relative to the incisal edges. Replicas were built with transparent epoxy resin (Redelease), which fully polymerized in approximately 48 hours, kept in an oven at 37°C. Incisal edges of the replicas were cut for subsequent analysis of the interface under the microscope. After cutting with a diamond disc, these incisal replicas were conditioned with 37% phosphoric acid and kept in an ultrasonic tank with 70% alcohol for 20 minutes in order to clean their surfaces, removing any debris. The replicas were evaluated using a Scanning Electron Microscope (SEM) (Jeol 5800), with a 500x magnification, by an examiner blind to the materials used, regarding the marginal sealing at the interface (presence/absence of marginal gap).
Fracture Strength Analysis
The specimens were evaluated for fracture resistance in a universal testing machine, where they were fixed in a horizontal position with the buccal surface facing downwards and the load was applied to the central point of the incisal third (2 mm from the incisal edge) by means of a wedge-shaped metal tip, with a crosshead speed of 1 mm/min. Fracture load was recorded in Newtons (N). Afterwards, the fractured specimens were analyzed for the type of fracture under a stereoscopic microscope (Kiowa). Fracture pattern analyzes were carried out at 40x magnification, and the failure mode was classified as: adhesive failure, located at the interface between the cementing agent and the tooth structure; cohesive failure of the ceramic, located in the laminate; cohesive failure of the substrate, located in the dental structure; and mixed failure, when there was more than one associated failure pattern.
Statistical analysis
Data were tabulated and subjected to statistical analysis, with a significant level of 5%. For the fracture resistance test, data were subjected to the Two-way ANOVA test, and for the marginal adaptation analysis and fracture patterns, the Chi square test was applied.
Results
Fracture Strength Analysis
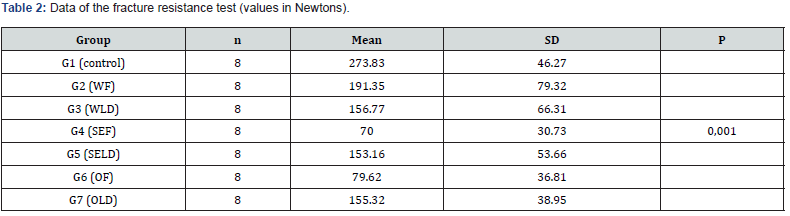
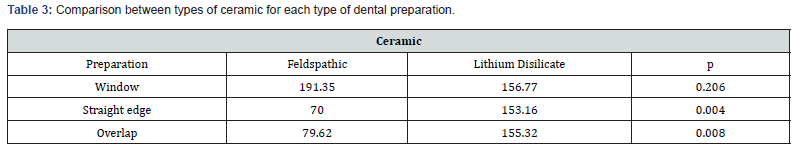
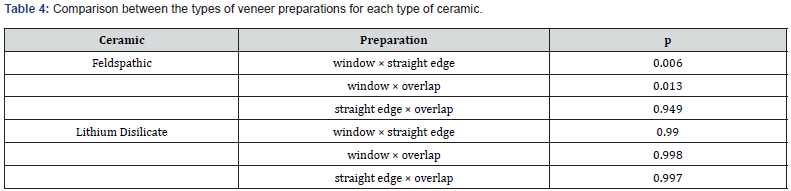
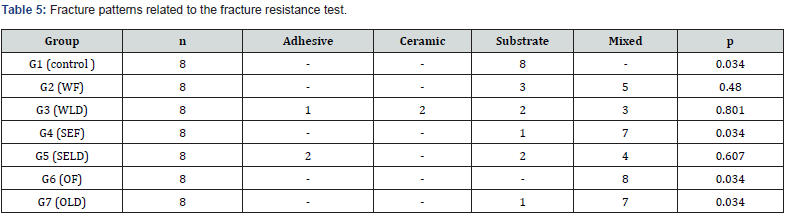
Data of the fracture resistance test were tabulated and subjected to statistical analysis using the Two-way ANOVA test, followed by Tukey’s multiple comparison test, with a significance level of 5%. The data passed the normality and equality of variance tests (Tables 2-4). Table 2 presents the average fracture loads (N) and standard deviation (SD) for each group. Analyzing the results based on the average of each group, the highest fracture resistance found was in the control group (sound teeth, 273.83N). The type of preparation (p=0.03) and the type of ceramic used (p=0.011) significantly influenced fracture resistance, as well as there was a significant interaction between the type of preparation and the type of ceramic (p=0.005). The control group was the one with the greatest resistance to fracture, being superior to all ceramic laminate techniques. When comparing the types of ceramic used, a statistically superior performance was obtained for the lithium disilicate ceramic, when the straight edges and overlap were present. Regarding the dental preparations, these showed a statistically significant difference within the feldspathic ceramics, being superior for the window. Table 5 shows the fracture patterns analyzed after fractures of the ceramic veneers. The Chi square test was performed, with a significant level of 5%. Groups 4, 6 and 7 showed a higher concentration of the fracture pattern in mixed failure.
Marginal Adaptation Analysis
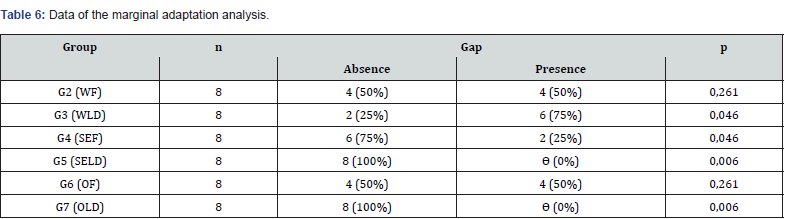
Data of the marginal adaptation of the veneers incisal replicas were tabulated and subjected to statistical analysis using the Chi square test, with a significance level of 5% (Table 6). The Qui square test demonstrated a statistically significant difference between groups, being groups 5 and 7 showing no marginal gaps (p=0.006), while groups 3 and 4 having 75% and 25% of gap presence, respectively (p=0.046).
Discussion
Ceramic veneers are aesthetic restorative procedures with high success and satisfaction rates in modern dentistry [3,6]. One of its greatest advantages is that the wear required on the dental structure is much less invasive and preserves a greater amount of tooth tissue when compared to the wear required to traditional crowns [17]. There are currently several types of ceramic systems that present excellent optical properties, allowing the restoration of aesthetics and function of teeth [4,18]. There are some variables that can directly influence the performance of ceramic veneers [10]. Therefore, two important variables were evaluated in this current study: the type of preparation (window, straight edge and overlap) and two different types of ceramic (feldspathic and lithium disilicate) [19]. Regarding fracture resistance analysis, the preparation design is one of the most controversial topics [16]. According to the same author, there are some types of failures that may arise over time, associated with this type of restoration, such as: fracture, decementation of the veneer and marginal leakage. Thus, in addition to fracture resistance and fracture patterns analysis, a scanning electron microscopic evaluation of the presence or absence of a marginal gap was carried out [20].
The results of the present study suggest that a windowtype preparation is ideally preferred for laminate veneer built with feldspathic ceramic. Data demonstrated that the fracture resistance of teeth with window-type preparations associated with feldspathic ceramic was greater than those with straight-edge or overlap preparations. The importance of preservation of the tooth structure is highlighted, as the window-type preparation, aiming less wear, restricted to the buccal surface, saving greater amount of dental tissue [2,5,10,11,16,17,21]. Castelnuovo et al. [22] discuss that the fracture resistance is provided mainly by the remaining tooth structure, and not by the retention capacity of the window preparation. On the other hand, for veneers built with lithium disilicate ceramic, the dental preparation did not influence the fracture resistance, even those with incisal reduction. As seen in a study by Chun et al. [23], the maximum fracture load was recorded for the control group. Furthermore, according to Schmidt et al. [14], the teeth in control group were fractured because the load was high enough to exceed the fracture threshold of the teeth. The masticatory force for upper anterior teeth was described by the same authors and it is close to 130 N, lower than the load values for the control group measured in the results of this current study.
The luting cement and bonding technique used is also extremely important for laminate veneers. To obtain clinical success and longevity for this type of restoration, cementation must be adhesive [6,24,25]. In addition, the importance of using lightcuring resin cement must be highlighted, because chemical or dual-setting resin cements can cause discoloration over time [6]. Furthermore, for Lin et al. [16], the thickness of the luting cement layer must be as thin and uniform as possible; it can affect the stress distribution at the interface between the luting cement and the veneer [26]. After the fracture resistance test, the analysis of the failure modes of the samples was carried out. In the control group, it was observed that the majority of teeth presented the fracture line at the cervical area of the tooth. For the overlap preparation groups, both the feldspathic and the lithium disilicate ceramic systems provided fractures involving the veneer itself. This fact may make it possible for the building of a new restoration, without compromising the tooth structure. According to Zarone et al. [8], cohesive ceramic fractures have occurred mainly at the incisal edge of the veneers, due to the greater stress in this region during function.
Regarding the marginal adaptation analysis, the technique of replicating specimens in epoxy resin was used [27]. The American Dental Association describes in its specifications for dental impression materials that polyvinyl siloxane must faithfully reproduce a 20 μm line. According to Petrie [28], the use of polyvinyl siloxane as an impression material is very reliable, due to its dimensional precision, stability, and other advantages, such as: excellent elastic recovery and good reproducibility of details. Epoxy resin also has several advantages, like minimal contraction, excellent copying capacity, hardness, resistance to abrasion, and stability to thermal cycles. The high fluidity of the epoxy resin allows the material to flow, penetrating all the details of the impression taking. Duke et al. [29] points out the epoxy resin as a material capable of providing precision in the reproduction of details, even reproducing a line of 1 to 2 μm. According to Lin et al [16] and Aschenbrenner et al. [20], replicated specimens analyzed under microscopy, in particular scanning electron microscopy, is a reliable method to evaluate the marginal adaptation of adhesive restorations.
The absence of an adequate marginal sealing between tooth and luting cement or luting cement and ceramic can lead to possible microleakage with bacterial penetration, hypersensitivity of the restored tooth and secondary caries (considering the size of the gap). Continuous cement margins are considered important for the longevity of the restorations, although no cementing material is always capable of promoting a perfect marginal sealing [20]. The superior performance of lithium disilicate ceramics is clear in this current study, in terms of fracture resistance and marginal sealing. When this type of ceramic was used, there was no influence of the type of dental preparation on fracture resistance. Therefore, ceramic veneers built with lithium disilicate ceramic are a choice that offers great aesthetics and optical properties, and better resistance [19,24]. Ceramic veneers associated with resin luting cement appear to be a viable and good option for restoring anterior teeth, in particular those built with lithium disilicate ceramic. However, in vitro analysis provides limited knowledge [16]. Therefore, clinical studies are needed to evaluate the performance of ceramic veneers, longitudinal, prospective or retrospective clinical trials, which would help to elucidate the best dental preparations and types of ceramic.
Conclusion
Within the results found in the present study, it is possible to
conclude that:
a) For feldspathic ceramic, the window preparation showed
better fracture resistance of the veneers.
b) For lithium disilicate ceramic, the type of dental
preparation did not influence the fracture resistance of the
veneers.
c) When the incisal edge is involved, laminate veneers built
with lithium disilicate ceramic associated with the straight edge or
overlap preparations showed no gap formation and had the best
fracture resistance.
References
- Araújo E, Perdigão J (2021) Anterior Veneer Restorations - An Evidence-based Minimal-Intervention Perspective. J Adhes Dent 23(2): 91-110.
- Stappert CFJ, Ozden U, Gerds T, Strub JR (2005) Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J Prosthet Dent 94(2): 132-139.
- Layton DM, Walton TR (2012) The up to 21-year clinical outcome and survival of feldspathic porcelain veneers: accouting for clustering. Int J Prosthodont 25(6): 604-612.
- Peumans M, Munck JD, Fieuws S, Lambrechts P, Vanherle G, et al. (2004) A prospective ten-year clinical trial of porcelain veneers. J Adhes Dent 6(1): 65-76.
- Nordbo H, Rygh-Thoresen N, Henaug T (1994) Clinical performance of porcelain laminate veneers without incisal overlapping: 3-year results. J Dent 22(6): 342-345.
- Calamia JR, Calamia CS (2007) Porcelain Laminate: reasons for 25 years of success. The Dent Clin N Am 51(2): 399-417.
- Akoglu B, Gemalmaz D (2011) Fracture resistance of ceramic veneers with different preparation designs. J Prosthodont 20(5): 380-384.
- Zarone F, Apicella B, Sorrentino R, Ferro V, Aversa R, et al. (2005) Influence of tooth preparation design on the stress distribution in maxillary central incisors restored by means of alumina porcelain veneers: A 3D-finite element analysis. Dent Mater 21(12): 1178-1188.
- Zarone F, Epifania E, Leone G, Sorrentino R, Ferrari M (2006) Dynamometric assessment of the mechanical resistance of porcelain veneers related to tooth preparation: A comparison between two techniques. J Prosthet Dent 95(5): 354- 363.
- Blunk U, Sabine Fischer, Jan Hajtó, Stefan Frei, Roland Frankenberger (2020) Ceramic laminate veneers: effect of preparation design and ceramic thickness on fracture resistance and marginal quality in vitro. Clin Oral Invest 24(8): 2745-2754.
- Smales RJ, Etemadi S (2004) Long-term survival of porcelain laminate veneers using two preparation designs: a retrospective study. Int J Prosthodont 17(3): 323-326.
- Meijering AC, Creugers NHJ, Roeters FJM, Mulder J (1998) Survival of three types of veneer restorations in a clinical trial: a 2.5-year interim evaluation. J Dent 26(7): 563-568.
- Nicholls JI (1988) Tensile bond of resin cements to porcelain veneers. J Prosthet Dent 60(4): 443-447.
- Schmidt KK, Chiayabutr Y, Phillips KM, Kois JC (2011) Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. J Prosthet Dent 105(6): 374-382.
- Nikzad S, Azari A, Dehgan S (2010) Ceramic (Feldspathic & IPS Empress II) vs. laboratory composite (Gradia) veneers; a comparison between their shear bond strength to enamel; an in vitro study J Rehabil 37(7): 569-574.
- Lin TM, Liu PR, Ramp RC, Essig ME, Givan DA, et al. (2012) Fracture resistance and marginal discrepancy of porcelain laminate veneers influenced by preparation design and restorative material in vitro. J Dent 40(3): 202-209.
- Edelhoff D, Sorensen JA (2002) Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent 87(5): 503-509.
- Quinn JB, Sundar V, Lloyd IK (2003) Influence of microstructure and chemistry on the fracture toughness of dental ceramics. Dent Mater 19(7): 603-611.
- Holand W, Schweiger M, Frank M, Rheinberger V (2000) A comparison of the microstructure and properties of the IPS Empress 2 and the IPS Empress glass-ceramics. J Biomed Mater Res 53(4): 297-303.
- Aschenbrenner CM, Lang R, Handel G, Behr M (2012) Analysis of marginal adaptation and sealing to enamel and dentin of four self-adhesive resin cements. Clin Oral Invest 16: 191-200.
- Hahn P, Gustav M, Hellwig E (2000) An in vitro assessment of the strength of porcelain veneers dependent on tooth preparation. J Oral Rehabil 27(12): 1024-1029.
- Castelnuovo J, Tjan AHL, Phillips K, Nicholls JI, Kois JC (2000) Fracture load and mode of failure of ceramic veneers with different preparations. J Prosthet Dent 83(2): 171-180.
- Chun YP, Raffelt C, Pfeiffer H, Bizhang M, Saul G, et al. (2010) Restoring strength of incisors with veneers and full ceramic crowns. J Adhe Dent 12(1): 45-54.
- Fradeani M (1998) Six-year follow-up with empress veneers. Int J Periodont Restor Dent 18(2): 217-225.
- Gresnigt M, Özcan M (2011) Esthetic rehabilitation of anterior teeth with porcelain laminates and sectional veneers. J Can Dent Assoc 77: b143.
- Magne P, Kwon KR, Belser UC, Hodges JS, Douglas WH (1999) Crack propensity of porcelain laminate veneers: a simulated operatory evaluation. J Prosthet Dent 81(31): 327-334.
- Chaffe NR, Bailey JH, Sherrard DJ (1997) Dimensional accuracy of improved dental stone and epoxy resin die materials. Part II: complete arch form. J Prosthet Dent 77(3): 235-238.
- Petrie CS (2003) Dimensional accuracy and surface detail reproduction of two hydrophilic vinyl polysiloxane impression materials tested under dry, moist, and wet conditions. J Prosthet Dent 90(4): 365-372.
- Duke (2000) Study of the physical properties of type IV gypsum, resin-containing, and epoxy die materials. J Prosthet Dent 83(4): 466-473.






























