Abstract
Intraoral precancerous lesions, such as leukoplakia and erythroplakia, often precede oral cancer and require early detection by healthcare professionals. To assess the knowledge and awareness of intraoral precancerous lesions among dental and medical students. A cross-sectional study was conducted using a structured questionnaire. A total of 232 responses were collected and analyzed descriptively. Findings were compared with prior literature. Most students demonstrated good theoretical knowledge—77.2% identified precancerous lesions correctly, and 90.9% chose biopsy as the best diagnostic method. However, only 21.6% correctly identified non-risk factors, indicating gaps in risk awareness. In this study students showed adequate knowledge overall, but misconceptions about risk factors and limited diagnostic exposure highlight the need for improved clinical training.
Keywords:Intraoral precancerous lesions; Eukoplakia; Erythroplakia; Oral submucous fibrosis; Dysplasia; Carcinoma in situ; Hyperkeratosis
Introduction
most common cancers worldwide. In South Asia, including India, it is a leading cause of cancer-related mortality, often linked to tobacco, areca nut, and alcohol consumption. However, most oral cancers are preceded by recognizable precancerous lesions that can be identified in their early stages. Intraoral precancerous lesions such as leukoplakia, erythroplakia, and oral submucous fibrosis are often asymptomatic but carry high malignant potential. Medical and dental students, being future healthcare providers, must be well versed in identifying these conditions. Several studies have shown that although students may possess theoretical knowledge, there is often a lack of diagnostic ability due to limited clinical exposure. This study aims to evaluate the awareness and knowledge level of dental and medical students regarding intraoral precancerous lesions and highlight areas that require academic reinforcement.
Materials And Methods
Study Design: A descriptive, cross-sectional study.
Participants: 232 medical and dental students, including final-year students (31.9%), CRRIs (40.9%), and postgraduates (27.2%).
Data Collection Tool: A structured Google Form questionnaire consisting of 10 close-ended questions focusing on knowledge, identification, diagnosis, and prevention of intraoral precancerous lesions.
Scoring: Responses were analyzed for correctness based on evidence from literature. Frequency and percentage of correct responses were calculated to assess overall awareness. No separate scoring rubric was applied, but knowledge adequacy was inferred from correct answer rates exceeding 70%.
Reference for Comparison
Key comparison was drawn from Ghimire [1], who studied knowledge, attitude, and diagnostic ability of oral cancer among students at Nepal Medical College.
As a result of scoring, out of 232 participants, the majority were CRRIs (40.9%).
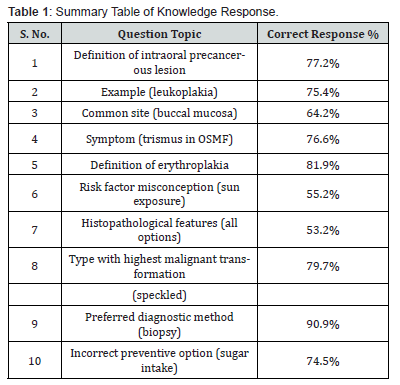
Knowledge Response
Definition of Precancerous Lesion: 77.2% correctly answered.
Example of Lesion: 75.4% identified leukoplakia.
Common Site: 64.2% selected buccal mucosa.
OSMF Symptom: 76.6% correctly answered trismus.
Erythroplakia Definition: 81.9% got it right.
Risk Factor Misconception: 55.2% incorrectly chose sun exposure as a risk factor.
Histopathology: 53.2% chose “all of the above” (dysplasia, carcinoma in situ, hyperkeratosis).
Most Malignant Type: 79.7% selected speckled leukoplakia.
Diagnostic Method: 90.9% chose biopsy.
Incorrect Preventive Strategy: 74.5% correctly selected “increased sugar intake.”
Results
Out of a total of 232 participants, the majority were CRRI students (40.9%), followed by final year students (31.9%) and postgraduates (27.2%). Dental and medical students were both included in the study, though subgroup data by field was not explicitly separated.
Knowledge Response
It was found that 77.2% of the students correctly identified intraoral precancerous lesions as those that may turn malignant. A large proportion (75.4%) recognized leukoplakia as the most common precancerous lesion. Regarding anatomical location, 64.2% responded that buccal mucosa is a common site for leukoplakia. When asked about symptoms of oral submucous fibrosis, 76.6% identified restricted mouth opening (trismus) as the primary symptom. A notable 81.9% of students correctly described erythroplakia as a red lesion with high malignant potential. However, misconceptions were observed regarding risk factors: only 21.6% correctly marked “high fiber diet” as not a risk factor, while 55.2% incorrectly considered sun exposure as one. Regarding histopathological diagnosis, 53.2% selected “all of the above,” acknowledging that leukoplakia may show hyperkeratosis, dysplasia, or carcinoma in situ. Most participants (79.7%) correctly identified speckled leukoplakia as having the highest malignant potential. An overwhelming 90.9% identified biopsy as the most accurate diagnostic method.
Attitude and Preventive Knowledge Response
In the question regarding preventive strategy, 74.5% correctly identified increased sugar intake as not a preventive method, suggesting a good level of understanding of effective prevention measures (Table 1).
Overall Findings
The results demonstrate adequate knowledge among the majority of respondents on key features of intraoral precancerous lesions. Clinical diagnostic confidence was not directly assessed in this section but inferred from correct identification of diagnostic methods (90.9% biopsy) and histopathological understanding (53.2%). Misconceptions in risk factor recognition suggest the need for reinforced education, especially regarding systemic factors versus local carcinogens.
Discussion
This study revealed that most students had a strong awareness of intraoral precancerous lesions, particularly in identifying leukoplakia and erythroplakia, aligning with findings from Ghimire [1] where over 70% demonstrated adequate knowledge. However, diagnostic confidence and clarity on risk factors remain areas of concern. Only 53.2% recognized the full histopathological spectrum of leukoplakia, and a significant number misidentified sun exposure as a risk factor. This mirrors similar gaps reported by Fotedar [2], Sitheeque [3]. The high percentage (90.9%) identifying biopsy as the diagnostic gold standard is encouraging and highlights theoretical preparedness, yet practical experience— such as performing or observing biopsies—is likely limited, as observed in prior studies. The variation in results suggests a disconnect between theory and practical exposure, possibly due to insufficient clinical postings or integration of oral pathology into the broader medical curriculum. The recommendations made in this study is to (i) Introduce Practical Workshops: Hands-on sessions on lesion identification, cytology, and biopsy techniques. (ii) Revise Curriculum: Integrate oral pathology more deeply into medical training. (iii) Promote Interdisciplinary Learning: Encourage medical-dental collaborative sessions. (iv) Mandate Clinical Postings: Ensure all students have exposure to oral oncology units. (v) Regular Seminars: Organize continuing dental and medical education (CDE/CME) on oral cancer [4-10].
Conclusion
This study concludes that while medical and dental students show good theoretical awareness of intraoral precancerous lesions, there are knowledge gaps regarding etiological risk factors and histopathological understanding. Clinical diagnostic exposure is presumed low and should be reinforced through curriculum updates.
References
- Ghimire (2022) Adequate knowledge but inadequate diagnostic ability was found among both dental and medical students.
- Fotedar (2015) Knowledge does not always translate into practice without clinical training.
- Sitheeque (2014) Dental students showed higher awareness of precancerous lesions compared to medical students.
- Baykul (2010) Early diagnosis is key to reducing oral cancer mortality.
- Hassona (2017) Lack of clinical exposure limits students’ diagnostic confidence.
- Warnakulasuriya (2009) Oral leukoplakia is the most common potentially malignant disorder.
- Gunjal (2020) Most students can identify leukoplakia but miss erythroplakia’s significance.
- Scully & Bagan (2008) Biopsy remains the gold standard for diagnosing oral precancer.
- Poudel (2020) Educational interventions significantly improve oral cancer awareness.
- Carter & Ogden (2007) Precancerous lesions are often asymptomatic, requiring trained eyes to detect them.






























