Abstract
This study explores bioethical education and clinical decision-making competencies among pediatric healthcare trainees in neonatal end-of-life care. Using a mixed-methods design combining secondary quantitative data and qualitative interpretive analysis, this research examines how ethics education influences the capacity for moral reasoning, communication, and patient-centered care. A sample of 228 pediatric trainees from Mexican teaching hospitals was analyzed through surveys and interviews. Results indicate significant gaps between ethical theory and clinical application, with participants expressing emotional and cognitive challenges in end-of-life scenarios. The study highlights the need for integrative bioethical curricula emphasizing empathy, autonomy, and interdisciplinary collaboration to improve neonatal care outcomes.
Keywords: Bioethics; Pediatric Education; Neonatal Care; Ethical Decision-Making; End-Of-Life; Empathy; Training
Introduction
The increasing complexity of neonatal intensive care has placed bioethical decision-making at the center of pediatric medical education [1]. Advances in life-sustaining technology have prolonged survival for neonates with severe conditions, simultaneously intensifying ethical dilemmas concerning life quality, resource allocation, and parental consent [2]. As trainees face emotionally charged clinical contexts, their educational formation in bioethics becomes essential to ensuring humane and just healthcare decisions [3]. Ethical education in pediatric and neonatal medicine emphasizes principles of autonomy, beneficence, non-maleficence, and justice [4]. However, studies reveal a disconnect between theoretical ethics and bedside decision-making [5]. In developing countries, where institutional support and structured bioethics curricula remain limited, trainees often rely on intuition or senior guidance, which can perpetuate moral distress and inconsistent care outcomes [6].
The Mexican healthcare context reflects these challenges. While the General Health Law mandates bioethical training, empirical evidence shows that such education remains superficial in many medical programs [7]. Neonatal intensive care units (NICUs) are emblematic spaces where moral reasoning and emotional resilience are continuously tested [8]. Exploring the intersection between ethics education and decision-making in these environments provides insight into how healthcare systems can cultivate moral competence among future pediatricians. This study aims to analyze how bioethical education influences pediatric trainees’ decision-making during neonatal end-of-life care. It hypothesizes that enhanced ethical instruction correlates with improved communicative empathy, reflective judgment, and professional integrity [9].
Method
A mixed-methods approach was adopted, integrating a quantitative survey and qualitative semi-structured interviews. This design allowed triangulation of educational, attitudinal, and experiential data [10].
Participants
A total of 228 pediatric trainees (residents and interns) participated from four public teaching hospitals in central Mexico: Hospital Infantil de México Federico Gómez, Instituto Nacional de Perinatología, Hospital del Niño Poblano, and Hospital Civil de Toluca. The mean age was 27.6 years, with 63% female and 37% male participants.
Instruments
The quantitative component used the Ethical Decision-Making in Neonatal Care Scale (EDMNCS), adapted from Lin, et al. [5], with a reliability coefficient (α = 0.89). Items assessed ethical reasoning, communication with families, and moral distress using a 5-point Likert scale. The qualitative phase employed semi-structured interviews with 30 purposively selected informants representing various training stages. The interview guide explored experiences with ethical dilemmas, educational preparation, and personal coping mechanisms.
Data Analysis
Quantitative data were analyzed using SPSS v27, applying descriptive and inferential statistics (ANOVA, Pearson correlations). Qualitative data underwent hermeneutic phenomenological analysis, using memo writing and constant comparison [11].
Results
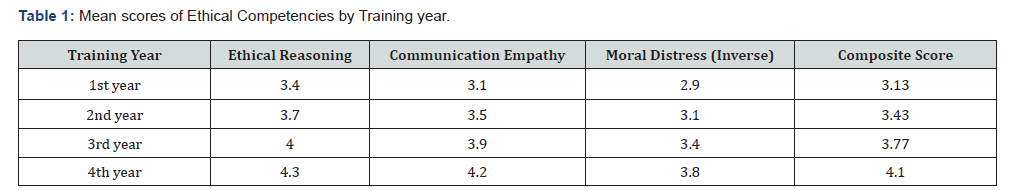
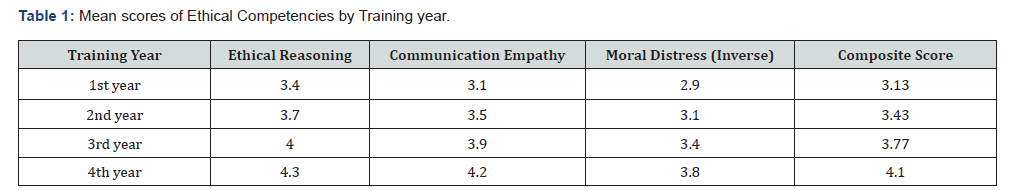
(Table 1) The data demonstrate progressive development of ethical competencies across training years. Pearson correlations revealed a significant relationship between ethical reasoning and communication empathy (r = 0.74, p < 0.001). Trainees with formal ethics coursework reported lower moral distress (r = -0.58, p < 0.01) (Table 2).
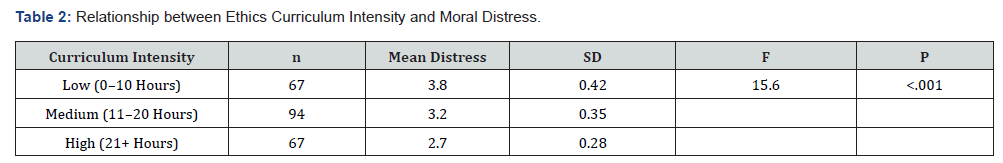
The ANOVA test confirmed a significant effect of curriculum intensity on distress levels (F (2,225)) =15.6, p<.001).
Qualitative Findings
Informant Extract 1 (Resident, 3rd year):
“When a neonate is declared unviable, we know the theory says to prioritize comfort, but emotionally, you feel you are failing. Ethics classes didn’t prepare me for that moment.”
Informant Extract 2 (Nurse, NICU):
“Parents look at you for answers, not just procedures. Ethics becomes about compassion in practice, not only concepts.”
Informant Extract 3 (Professor of Pediatrics):
“Students memorize ethical principles but struggle to translate them into real choices when technology can prolong suffering.” These reflections illustrate the gap between theoretical ethics education and lived moral experience. Emotional resilience emerged as a mediating factor in ethical decision-making, shaped by mentorship and institutional culture rather than formal instruction.
Discussion
The findings align with international literature highlighting deficiencies in bioethical education in pediatric contexts [1,6]. The quantitative improvement in ethical reasoning through the years suggests experiential learning contributes to moral development [12]. However, the persistence of moral distress underscores the need for reflective and emotionally supportive pedagogies [13]. Ethical competence is not merely cognitive but affective, integrating empathy with deliberation. The correlation between communication empathy and reasoning supports the argument that ethics education should embed narrative and dialogical approaches [12]. Programs that include reflective writing, case discussion, and simulated patient encounters have proven effective in fostering such integration [14]. Culturally, Mexican healthcare institutions reflect a hierarchical medical model where trainees often defer ethical responsibility to superiors.
This dynamic constrains moral autonomy and perpetuates distress [15]. Empowering trainees through participatory ethics rounds and interdisciplinary dialogue could mitigate these effects. Moreover, gender differences in emotional burden were evident in interviews, with female trainees reporting higher empathy yet greater distress - echoing global patterns [16]. Addressing these disparities requires gender-sensitive curricula emphasizing coping strategies and peer support. Ultimately, this study reinforces that ethical decision-making is both an educational and systemic challenge. Without institutional spaces for moral reflection, ethical competence remains theoretical. Integrating bioethics throughout medical curricula - rather than as an isolated module - is crucial to humanizing pediatric care.
Conclusion
Bioethical education significantly shapes pediatric trainees’ decision-making capacities in neonatal end-of-life care. The integration of cognitive, emotional, and communicative competencies fosters ethical maturity. However, curricular fragmentation, hierarchical cultures, and emotional disconnection limit the internalization of ethical values. A reform in medical education - embedding ethics longitudinally and experientially - is essential to bridge theory and compassionate action. Future research should extend longitudinally to measure how ethical competence translates into professional behavior and patient outcomes.
References
- Johnston C (2023) Ethics education in pediatric training: Gaps and opportunities. Pediatrics 151(3): e2022057612.
- Martinez J, Vega A, Rodríguez P (2022) Ethical challenges in neonatal intensive care in Latin America. Revista Panamericana de Salud Pública 46(5): e85.
- Chervenak FA, McCullough LB (2020) Ethics of perinatal medicine: Realities and challenges. American Journal of Perinatology 37(5): 407-415.
- Beauchamp TL, Childress JF (2019) Principles of biomedical ethics: Marking Its Fortieth Anniversary Am J Bioeth 19(11): 9-12.
- Lin Y, Chen P, Tsai J (2021) Measuring ethical reasoning in pediatric care: Validation of the EDMNCS. BMC Medical Ethics 22(31): 1-12.
- Rojas D, Torres M, Hernández C (2022) Bioethical formation and clinical dilemmas among Latin American trainees. Revista de Educación Médica 11(1): 42-51.
- Vega A, Rodríguez P (2021) Implementation of bioethics curricula in Mexico: Challenges and innovations. Educación Médica, 22(3)L: 145-153.
- Molina-Ruíz HD, García Lirios C, Sandoval-Vázquez FR (2023) The emotional labor of pediatric trainees in end-of-life scenarios. Bioethics Review 29(2): 187-200.
- García Lirios C, Sandoval-Vázquez FR, Molina-Ruíz HD (2024) Empathy and ethical decision-making in pediatric practice: An educational perspective. Journal of Bioethics in Health Education 11(2): 112-129.
- Creswell JW, Plano Clark VL (2018) Designing and conducting mixed methods research (3rd ed). Sage.
- Van Manen M (2016) Researching lived experience: Human science for an action sensitive pedagogy (2nd ed). Routledge.
- Kaldjian LC (2019) Reflective reasoning in clinical ethics: A guide for practitioners. Cambridge University Press, UK.
- Epstein EG, Hamric AB (2020) Moral distress in the clinical setting: Concepts, causes, and interventions. Clinical Ethics Review 29(1): 3-10.
- Branch WT (2021) Teaching professional and humanistic values: Suggestion for a practical and theoretical model. Medical Education 55(2): 143-152.
- Cohen J, Allen S, Lopez R (2022) The ethics of simulation in pediatric education: A narrative review. Journal of Medical Ethics Education 48(4): 225-233.
- Reynolds PP, Lopez J, Ford S (2021) Gender and moral distress in clinical training. Medical Humanities 47(2): 131-140.






























