Mobile Posturography for the Assessment of Balance and Risk of Falling in Parkinson’s Disease: A Review
Júlia Lana Fonseca1, Mario Edvin Greters1 and Gisele Mara Silva Gonçalves2*
1Faculty of Medicine - Pontifical Catholic University of Campinas, Brazil
2Postgraduate Programme in Health Sciences, Pontifical Catholic University of Campinas, Brazil
Submission: November 22, 2023; Published: December 12, 2023
*Corresponding author: Gisele Mara Silva Gonçalves, Postgraduate Programme in Health Sciences, Pontifical Catholic University of Campinas, Brazil
How to cite this article: Júlia Lana F, Mario Edvin G, Gisele Mara Silva G. Mobile Posturography for the Assessment of Balance and Risk of Falling in Parkinson’s Disease: A Review . Glob J Oto, 2023; 26(3): 556187. DOI: 10.19080/GJO.2023.26.556187
Abstract
Purpose: Conduct a review of clinical studies that applied balance tests and posturography in patients with Parkinson’s disease and potential use of these tools for preventing falls.
Research Strategy: Integrative literature review guided according to Prisma protocol guidelines.
Selection Criteria: Clinical trials that evaluated the use of mobile posturography and platform posturography equipment and that performed the “Timed Up and Go” test was included. There were not any limits regarding language or year of publication.
Data analysis: The retrieved studies were submitted to the eligibility criteria and those included were read and analyzed.
Results: Only seven studies were eligible and included in the final sample. They demonstrated that mobile posturography and platform posturography, although used in the assessment of several clinical situations, are still little explored in Parkinson’s disease.
Conclusion: Mobile posturography performed with Vertiguard® using the Standard Balance Deficit Test proved to be one of the most efficient tools for predicting patients with Parkinson’s Disease at greater risk of falling, and it is also useful for the rehabilitation of these patients.
Keywords: Gait analysis; Parkinson disease; Postural balance; Sensory; Neurofeedback
Abbreviations: PD: Parkinson’s Disease; UPDRS Unified Parkinson’s Disease Rating Scale; ABC: Activities-Specific Balance Confidence; CDP: Computer Dinamycs Posturograph; DHI: Dizziness Handicap Inventory; LOS: Limits of Stability; SBDT: Standard Balance Deficit Test; SOT: Sensorial Organization Test; TUG: Timed Up and Go
Introduction
Parkinson’s disease (PD) is one of the most prevalent neurodegenerative diseases and causes progressive motor and non-motor impairments in the affected individual’s movements [1]. Postural instability is one of the most debilitating motor symptoms [1] and it results from the loss of reflexes that maintain the orthostatic position, trunk rotation and flexed posture [2]. For this reason, it is associated with an increased risk of falling, which can result in complications such as fractures, reduced mobility and self- restriction of activities due to fear of falling and reduced quality of life [1]. Generally, postural instability presents itself in more advanced stages (from stage three onwards in the Hoehn and Yahr classification, which consists of stages from zero to five, with three classified as moderate disability, and four and five classified as severe disability) of PD [1,3]. Patients known as “fallers”, which are those who have had at least one fall in the last three to six months, usually have PD for a longer time and have severe disease [4].
In these patients, symptoms such as motor fluctuations, dyskinesia and freezing are also more common [4]. Bradykinesia and rigidity respond to dopamine treatment and affect balance and gait since the beginning of the disease [3]. However, impairment in kinaesthesia, lack of automatism and executive function dysfunction occur later in the disease and are not responsive to dopamine [3]. Changes in gait, which can impact on balance, such as bradykinetic steps, result in increased dependence on vision to compensate for the postural movement [3,2]. The clinical assessment of postural instability in PD is usually carried out using the retropulsion test, but it is difficult to standardise [1] and its ability to predict the risk of falls is questioned [2]. It has been shown that the Unified Parkinson’s Disease Rating Scale (UPDRS) and the body sway area are independent and important risk factors for predicting the risk of falling [4].
In PD, postural instability is evident both at rest and when performing activities [1]. As such, a quantitative assessment of postural instability can be made using posturography, which allows balance to be assessed both statically and dynamically [1]. Based on the premise that posturography helps assess balance and the risk of falls in PD patients and can be used to prevent falls, the aim of this study was to review clinical studies that applied balance tests and posturography in PD.
Methods
The review was based on the research question “Is assessing individuals with Parkinson’s disease for balance and falls risk using balance tests and gait posturography effective for clinical guidance on falls risk and prevention?”. The research protocol was registered in the International Prospective Register of systematic reviews (PROSPERO): CRD42023464490. The search was carried out in April 2023 on the CAPES Journal Portal (https://www-periodicos-capes- gov-br.ezl.periodicos.capes. gov.br/index.php?), which is a virtual library that gathers and makes available international scientific production to research institutions in Brazil, covering the main databases in the health area, such as Embase, PubMed, Scopus, ScienceDirect and Scielo. Two combinations of descriptors indexed on the Medical Subject Heading (MeSH), Health Sciences Descriptors (DeCS) and Embase Subject Headings (Emtree) platforms were used: “Parkinson AND Vertiguard” and “Parkinson AND mobile posturography”.
Clinical trials that evaluated the use of gait posturography and platform posturography equipment and that carried out the “Timed Up and Go” test were included, with no limits as to language or year of publication. We excluded review articles, book chapters, letters to the editor and other types of scientific literature, studies that did not use posturography and studies in which the study population did not include Parkinson’s disease. The studies retrieved were subjected to selection criteria and the elimination of duplicate articles and those that did not meet the eligibility criteria; the studies were read in full, and the information extracted and collated in a table for later analysis, in order to meet the proposed objectives.
Results
The search resulted in nine articles being retrieved and after applying the inclusion and exclusion criteria, the final sample consisted of seven articles (Figure 1). The results of the studies analyzed are shown in (Table 1).
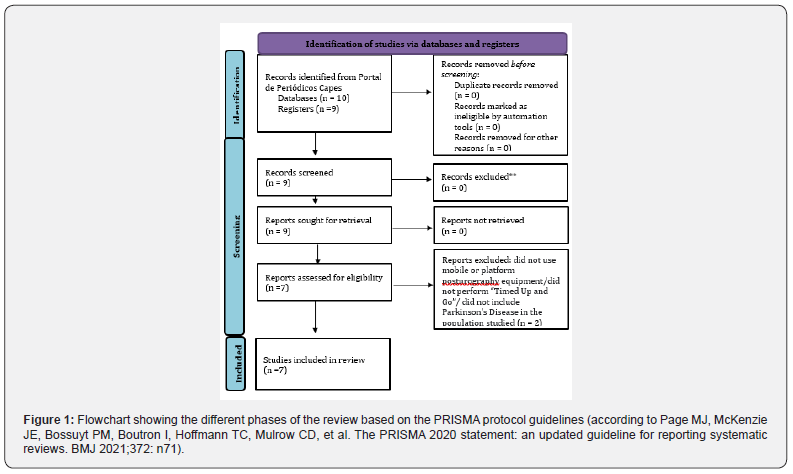
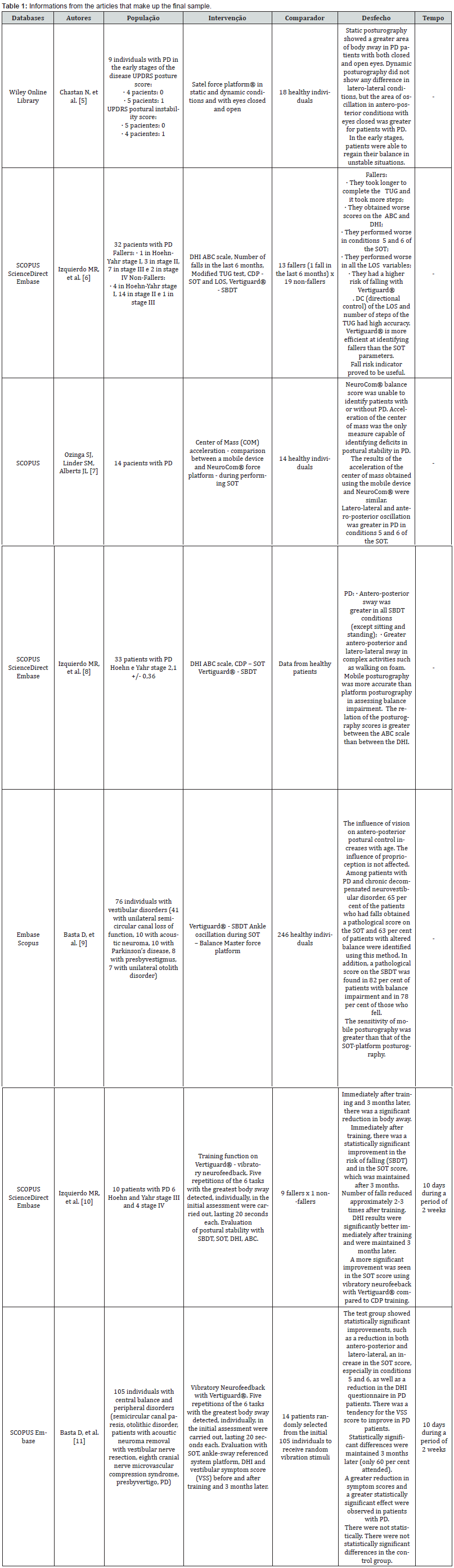
Table Abbreviations: TI: Time not Informed; ABC: Activities-Specific Balance Confidence; CDP: Computer Dinamycs Posturography; DHI: Dizziness Handicap Inventory; LOS: Limits of Stability; SBDT: Standard Balance Deficit Test; SOT: Sensorial Organization Test; TUG: Timed Up and Go; UPDRS: Unified Parkinson’s Disease Rating Scale.
Discussion
The evaluation of the application of posturography in Parkinson’s Disease (PD) was the motivation for this review. Posturography is a method for assessing the balance of individuals with Parkinson’s disease, as well as predicting which patients are at greater risk of falling. In a study in which the intervention with nine patients involved Satel Force Platform posturography® in static and dynamic conditions, with eyes closed and open, it was shown that postural instability is present since the early stages of PD, mainly at rest [5]. In the early stages of the disease, the ability to control balance during movement is not affected yet, apparently [5].
In a study of 32 participants with PD, 13 of them had fallen at least once in the last six months and were the worst performers in the modified Timed Up and Go (TUG) test, in conditions five and six of the Sensorial Organisation Test (SOT), in the Limits of Stability Balance Test (LOS), as well as they had the highest risk of falling in the Standard Balance Deficit Test (SBDT) with Vertiguard® [6,7]. Three studies have shown superior sensitivity in identifying the risk of falling using the SBDT- Vertiguard® compared to the SOTplatform posturography [6,8,9]. The SBDT identified 82 per cent of patients with balance disorders and 70 per cent of those who fell, while the SOT identified 63 per cent of patients with balance disorders and 65 per cent of those who fell [9]. The sensitivity of the SOT was 54.5 per cent and that of the SBDT was 93.9 percent [8].
In addition, a greater association has been shown between the result obtained with the Vertiguard® in relation to the Activitiesspecific Balance Confidence scale (ABC) than the Dizziness Handicap Inventory (DHI) - the last two tests are subjective scores that make it possible to assess the level of confidence in carrying out activities without losing balance and the impact of dizziness on quality of life, respectively [8]. SBDT through the use of the Vertiguard® makes it possible to assess body sway in the free field and in dynamic situations, situations in which falls occur in PD. It also makes it possible to assess lateral sway, which is common in PD, possibly due to rigidity [8]. In addition, the “risk of falling” indicator provided by the SBDT has proved useful for identifying individuals who have fallen [6].
The measurement of the acceleration of the center of mass can be assessed using the NeuroCom Smart Balance Master® or using a mobile electronic device with similar results during the SOT, and this parameter is capable of identifying postural stability deficits in PD, which the SOT balance score cannot [7]. Furthermore, it was observed that in conditions where vision was not available or somatosensory information was inconsistent, as in SOT activities five and six, individuals with PD showed greater postural instability compared to healthy individuals, reinforcing the proposal that individuals with PD rely more on vision to maintain balance in order to try to compensate for the loss of somatosensory feedback [7]. In addition, the larger body sway area with closed eyes in dynamic situations suggests that PD patients rely mainly on vision for postural control [5]. Postural instability in PD results from impaired visual and vestibular processing [10].
Another application of the Vertiguard® equipment, apart from its use in assessing balance and the risk of falling, is in the rehabilitation of PD patients through vibratory neurofeedback [10,11]. In one study [11], the test group showed statistically significant improvements, such as a reduction in both anteroposterior and latero-lateral trunk sway, an increase in the SOT score, especially in conditions five and six, as well as a reduction in the DHI questionnaire result in PD patients. There was a tendency for vestibular symptom scores to improve in PD patients [11]. This is important since postural instability does not improve with the use of dopaminergic medication and, often, conventional rehabilitation with physiotherapy, for example, does not have significant and lasting results. Furthermore, vibratory neurofeedback allows for individualized training [10]. The two studies analysed showed an improvement in the risk of falling (SBDT) immediately after training and this was maintained three months later [10,11]. The number of falls decreased between two to three times and the DHI result remained well after three months [10]. Training with Computer Dynamic Posturography (CDP) did not produce results as significant as those of vibratory neurofeedback (Vertiguard®) [10].
Conclusion
Mobile posturography using Vertiguard®, applying the Standard Balance Deficit Test, has proved to be one of the most efficient tools for predicting which PD patients are at most risk of falling. It allows these patients to be assessed in a free field, better simulating how falls occur. In addition, the Vertiguard® can be used in the rehabilitation of PD patients using vibratory neurofeedback which, until now, has proved to be effective and quick to perform, with long-lasting results in postural stability. The limitations of this study include the limited number of studies published until the date on this subject, which were carried out with a small sample population. The applications of posturography have proved to be an area for further study in the future.
Acknowledgements
Pontifícia Universidade Católica de Campinas (PUC-Campinas) pela bolsa de Iniciação Científica.
References
- Crouse JJ, Phillips JR, Jahanshahi M, Moustafa AA (2016) Postural instability and falls in Parkinson’s disease. Revi Neurosci 27(5): 549-555.
- Lena F, Modugno N, Greco G, Torre M, Cesarano S, et al. (2023) Rehabilitation interventions for improving balance in Parkinson’s disease: a narrative review. Am J of Phys Med Rehabil 102(3): 270-274.
- Park JH, Kang YJ, Horak FB (2015) What Is Wrong with Balance in Parkinson’s Disease? J Mov Disord 8(3): 109-114.
- Matinolli M, Korpelainen JT, Korpelainen R, Sotaniemi KA, Matinolli VM, et al. (2009) Mobility and balance in Parkinson’s disease: a population-based study. Eur J Neurol 16(1): 105-111.
- Chastan N, Debono B, Maltête D, Weber J (2008) Discordance between measured postural instability and absence of clinical symptoms in Parkinson’s disease patients in the early stages of the disease. J Mov Disord 23(3): 366-372.
- Rossi-Izquierdo M, Basta D, Rubio-Rodríguez JP, Santos-Pérez S, Ernst A, et al. (2014) Is posturography able to identify fallers in patients with Parkinson’s disease? Gait Posture 40(1): 53-57.
- Ozinga SJ, Linder SM, Alberts JL (2017) Use of Mobile Device Accelerometry to Enhance Evaluation of Postural Instability in Parkinson Disease. Am J of Phys Med Rehabil 98(4): 649-658.
- Rossi-Izquierdo M, Soto-Varela A, Ernst A, Rubio-Rodríguez JP, Santos-Pérez S, et al. (2016) What Could Posturography Tell Us About Balance Problems in Parkinson’s Disease? Otol Neurotol 37(9): 326-331.
- Basta D, Rossi-Izquierdo M, Soto-Varela A, Ernst A (2013) Mobile Posturography: Posturographic Analysis of Daily-Life Mobility. Otol Neurotol 34(2): 282-297.
- Rossi-Izquierdo M, Ernst A, Soto-Varela A, Santos-Pérez S, Faraldo-García A, et al. (2013) Vibrotactile neurofeedback balance training in patients with Parkinson’s disease: Reducing the number of falls. Gait Posture 37(2): 195-200.
- Basta D, Rossi-Izquierdo M, Soto-Varela A, Greters ME, Saraiva R, et al. (2011) Efficacy of a Vibrotactile Neurofeedback Training in Stance and Gait Conditions for the Treatment of Balance Deficits. Otol. Neurotol 32(9): 1492-1499.





























