Acute Myocardial Infarction as a First Manifestation of Thyrotoxicosis
Lynnie Oberg Arouca1, Tibério Augusto Oliveira Costa1, Jose Eduardo Camargo Ribeiro Filho1,2 and Murillo de Oliveira Antunes1,2*
1Hospital Universitário São Francisco (HUSF), Brazil
2Universidade São Francisco (USF), Brazil
Submission: December 02, 2019;Published: January 22, 2020
*Corresponding author: Murillo de Oliveira Antunes, Hospital Universitário São Francisco (HUSF), Brazil
How to cite this article:Lynnie Oberg Arouca, Tibério Augusto Oliveira Costa, Jose Eduardo Camargo Ribeiro Filho, Murillo de Oliveira Antun. Acute Myocardial Infarction as a First Manifestation of Thyrotoxicosis. J Cardiol & Cardiovasc Ther. 2020; 15(5): 555921. DOI: 10.19080/JOCCT.2020.15.555921
Abstract
Thyrotoxicosis is a clinical condition that results from overproduction of triiodothyronine, thyroxine or both. Currently, there is very consistent evidence that thyrotoxicosis is directly associated with the presence of a prothrombotic state, considering that a high T3 concentration is associated with a 2.6 times higher probability of coronary events. We report a case of Acute Myocardial Infarction (AMI), in a young patient with no risk factors for coronary disease and hyperthyroidism
Keywords:Hyperthyroidism; Angina Pectoris; Thrombosis
Case Report
A 34-year-old male patient, with a history of precordial pain in severe tightness, accompanied by irradiation to the upper left limb, with sudden onset 3 hours earlier. The patient denies comorbidities, continuous medication uses and licit or illicit drug use. As a family history, father treated hyperthyroidism for 7 years. On physical exam, the patient was only tachycardic (heart rate 120 bpm), with no other significant changes. The electrocardiogram showed ST-segment elevation in an extensive anterior wall (Figure 1).
Drug therapy for acute coronary syndrome was initiated and the patient underwent coronary angiography, which showed the presence of obstructive lesion of the Anterior Descending (AD) artery, with large thrombotic load and then underwent primary angioplasty (Figure 2).
Later, the echocardiogram showed 40.2% ejection fraction, moderate left ventricular segmental involvement with apical thrombus. The patient remained tachycardic during hospitalization, despite optimized doses of the β-blocker. Thus, a new clinical history was taken from the patient, who reported palpitations, significant weight loss, excessive sweating and heat intolerance in the last 60 days, and thyrotoxicosis was suspected. Renal function, lipid and glycemic profile were normal. During the investigation of the case thrombophilias were discarded. The measurement of thyroid function showed TSH 0.01 μUI/ml, fT4 4.92 ng/dl and T3 2.12 ng/dl, confirming the diagnosis (Table 1). The patient underwent thiamazole treatment, with significant improvement in thyroid profile and clinical symptoms.
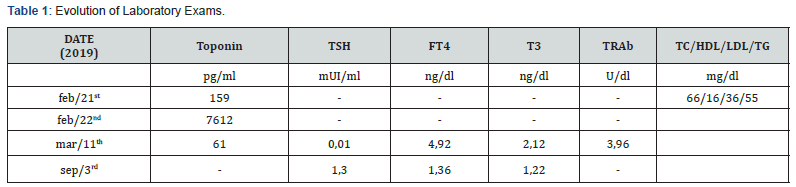
TSH: Thyroid-stimulating hormone; FT4: Free thyroxine; T3: Triiodothyronine, TRAb: anti-TSH receptor antibody; TC: Total cholesterol; HDL: High density lipoprotein; LDL: Low density lipoprotein; TG: Triglycerides.
Discussion
AMI can occur in young subjects, and could be related to risk factors as hyperlipidemias, hypercoagulable states, cocaine abuse and other factors. It however, still relatively rare in young people [1]. Thus in patients without coronary risk factors, other causes of AMI should be investigated, including thyroid disfunction.
There is evidence that thyrotoxicosis is directly associated with the presence of a prothrombotic state [2, 3]. Several coagulation and fibrinolytic parameters appear to be affected by thyrotoxicosis. For example, higher concentrations of procoagulant factors as prothrombin, fibrinogen, factor VIII, factor IX and von Willebrand factor can occur [2,4,5].
On the other hand, we observe a lower fibrinolytic activity as a consequence of increased levels of plasminogen activator inhibitor-1 and decreased levels of anticoagulant factors, such as protein C and the plasmin-antiplasmin complex during the period of hyperthyroidism [2,6,7].
Long-term follow-up studies have revealed that the past history of overt hyperthyroidism have an increased mortality from cardiovascular and cerebrovascular disease [8]. The same was verified in those with subclinical hyperthyroidism [9]. Another study associated the elevated serum free triiodothyronine (fT3) concentration with a 2.6-fold greater likelihood of the presence of a coronary event [10].
In this case report, the subject did not have any typical coronary risk factors. Regarding its personal history, also had no comorbidities or was on continuous medication. The serum cholesterol levels were within the expected range (Table 1), and there was no history of illicit adrenergic stimulant drug use. In addition, the patient had symptoms compatible with a metabolic hyperactivity syndrome. Considering this scenario, associated with the acute event characteristic of a state of hypercoagulability, the hypothesis of thyrotoxicosis was then raised, which was confirmed positive later. Thrombophilias were discarded.
Conclusion
Hyperthyroidism may be associated with the development of Acute Coronary Syndrome, by its prothrombotic state. Thus, awareness is needed for the possibility of such serious complications in patients with hyperthyroidism. Therefore, young patients without risk factors for coronary artery disease should be investigated.
References
- Zarich S, Luciano C, Hulford J, Abdullah A (2006) Prevalence of metabolic syndrome in young patients with acute MI: does the Framingham Risk Score underestimate cardiovascular risk in this population? Diab Vasc Dis Res 3(2): 103-107.
- Squizzato A, Romualdi E, Büller HR, Gerdes VE, et al. (2007) Clinical review: Thyroid dysfunction and effects on coagulation and fibrinolysis: a systematic review. J Clin Endocrinol Metab 92(7): 2415-2420.
- Vescovi PP, Favaloro EJ, Lippi G, Garofano M, Montagnana M, et al. (2011) The spectrum of coagulation abnormalities in thyroid disorders. Semin Thromb Hemost 37(1): 7-10.
- Arnaout MA, Awidi AS, el-Najdawi AM, Khateeb MS, Ajlouni KM (1992) Arginine-vasopressin and endothelium-associated proteins in thyroid disease. Acta Endocrinol 126(5): 399-403.
- Van Zaane B, Squizzato A, Debeij J, Dekkers OM, Meijers JC, et al. (2011) Alterations in coagulation and fibrinolysis after levothyroxine exposure in healthy volunteers: a controlled randomized crossover study. J Thromb Haemost 9(9): 1816-1824.
- Stuijver DJ, van Zaane B, Romualdi E, Brandjes DP, Gerdes VE, et al. (2012) The effect of hyperthyroidism on procoagulant, anticoagulant and fibrinolytic factors: a systematic review and meta-analysis. Amsterdam 108(6): 1077-1088.
- Lewandowski KC, Rechciński T, Krzemińska-Pakuła M, Lewiński A (2010) Acute myocardial infarction as the first presentation of thyrotoxicosis in a 31-year old woman - case report. Thyroid Res 3(1): 1.
- Franklyn JA, Maisonneuve P, Sheppard MC, Betteridge J, Boyle P, et al. (1998) Mortality after treatment of hyperthyroidism with radioactive iodine. N Engl J Med 338(11): 712-718.
- Parle JV, Maisonneuve Ing P, Sheppard MC, Boyle P, Franklyn JA, et al. (2001) Prediction of all cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: a 10-year cohort study. Lancet 358(9285): 861-865.
- Peters A, Ehlers M, Blank B, Exler D, Falk C, et al. (2000) Excess triiodothyronine as a risk factor of coronary events. Arch Intern Med 160(13): 1993-1999.






























