Cerebellar Ischemic Stroke as a Complication of an Acute Coronary Syndrome: Case Report
Abdul Hakeem M*, Harouna S, Fadoul A, Arous S, Benouna M.EG, Drighil A, Azzouzi L and Habbal R
Department of cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
Submission: May 26, 2021;Published: June 09, 2021
*Corresponding author: Abdul Hakeem Marwa, Department of cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
How to cite this article:Abdul Hakeem M, Harouna S, Fadoul A, Arous S, Benouna M, Drighil A, et al. Cerebellar Ischemic Stroke as a Complication of an Acute Coronary Syndrome: Case Report. J Cardiol & Cardiovasc Ther. 2021; 17(1): 555955. DOI: 10.19080/JOCCT.2021.17.555955
Abstract
Stroke represents an enormous public health problem. Its cardioembolic origin is not negligible and represents approximately 30% of etiologies of which, approximately 2.2% are imputable to the acute coronary syndrome. Acute cerebellar ischemic events are rarely reported in the literature.
We report the case of a cerebellar ischemic stroke occurring 48 hours after a ST segment elevation myocardial infarction.
Keywords:Acute cerebrovascular events; Cerebellar ischemic stroke; Acute coronary syndrome
Introduction
Cardiovascular diseases (CVD) are the most common cause of death in the world, representing more than 17 million deaths per year, with coronary heart disease accounting for half of them [1,2].
Stroke is the third leading cause of death and the leading cause of major disability worldwide. It is an uncommon complication during and after acute coronary syndrome (ACS), however, it is associated with a significant increase in morbidity and mortality. Thus, the incidence of strokes during the in-hospital phase of ACS varies between 0.7% and 2.2%, its in-hospital and 1-year mortality is of 30.1% and 36.5%, respectively, and this is despite improved reperfusion strategies and management of cardiovascular risk factors [3,4]. The incidence of stroke is highest in the first few days after ACS and gradually decreases with time [3,5].
The aim of this observation is to report the case of a patient presenting a cerebellar ischemic stroke 48 hours after an acute myocardial infarction.
Case Report
A 52-year-old male presented a sudden onset of chest pain 4 hours prior to his admission to the intensive care unit at the cardiology department of Ibn Rochd university hospital of Casablanca. The patient had multiple cardiovascular risk factors: type 2 diabetes treated with insulin, hypertension managed by calcium channel blocker and smoking.
On clinical examination, the patient was conscious; he didn’t experience any syncope, he didn’t have any motor or sensory deficit. His blood pressure was 101/67mmhg; his heart rate was at 58 beats per minute, with normal auscultation and without signs of heart congestion. The ECG revealed a ST-segment elevation in the inferior leads, with ST segment depression in leads V3 to V6 and a second-degree type 2 atrioventricular block.
A primary percutaneous coronary intervention (PCI) was urgently performed; a drug-eluting stent was placed in the right coronary artery, with TIMI 3 flow. Subsequently, the symptoms subsided and the AV block receded.
Transthoracic echocardiography revealed an abnormal left ventricle’s segmental wall motion, with an ejection fraction of 30% estimated by the biplane method, filling pressures were not elevated; there were no signs of valvular disease, the right ventricle had a good systolic longitudinal function, the inferior vena cava was not dilated and there was no pericardial effusion.
The patient received a double antiplatelet therapy (Aspirin 75mg, Clopidogrel 75mg), Atorvastatin 80mg and small dosages of ACE inhibitor.
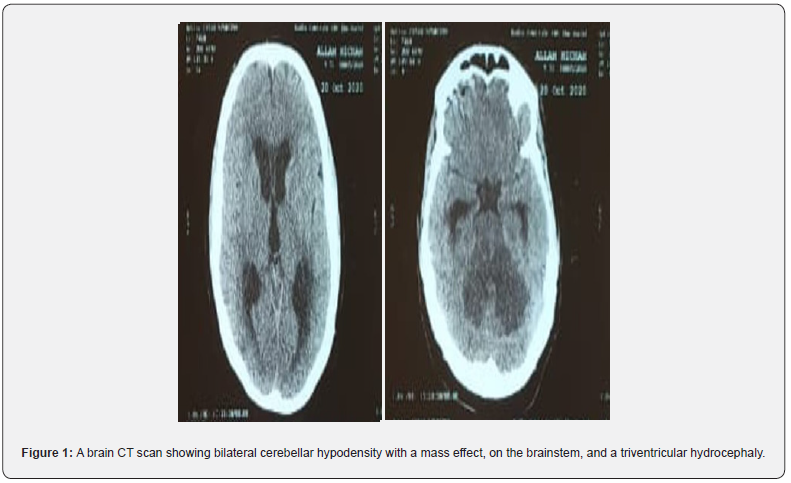
Forty-eight hours afterwards, the patient presented a bilateral cerebellar syndrome with internal gaze paralysis on the right eye with no swallowing difficulties. A brain CT scan was performed showing bilateral cerebellar hypodensity with a mass effect, on the brainstem, and a triventricular hydrocephaly (Figure 1). An MRI (magnetic resonance imaging) was conducted, revealing a bilateral, subacute, superior cerebellar artery infarction without any abnormalities on the MR angiography (MRA) (Figure 2) with petechial hemorrhage on the right cerebellar hemisphere (Not shown). The 24-hour Holter monitoring showed no episodes of atrial fibrillation (AF). The supra-aortic trunks echo-doppler (TSA) didn’t display any signs of significant stenosis.
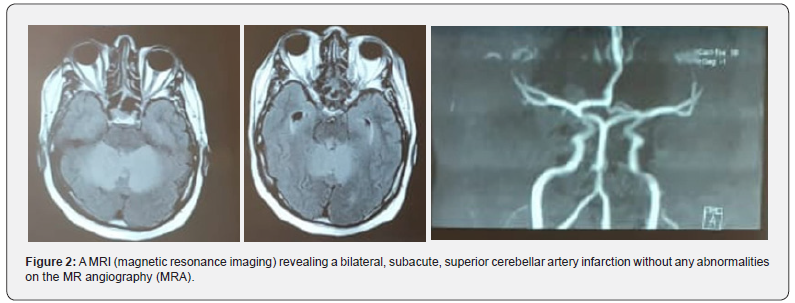
Due to the hemorrhagic transformation discovered on MRI, one antiplatelet treatment was withdrawn and only Clopidogrel was maintained. The patient also received a mannitol infusion to manage the mass effect. A CT scan performed 48 hours later showed the same findings with no worsening of the hemorrhagic infarction. The patient’s clinical state did not exacerbate, therefor, a decompressive craniectomy was not indicated.
The patient was discharged from the hospital on the 12th day of admission with a close follow-up appointment in consultation.
Discussion
Atherosclerosis is a diffuse and progressive pathophysiological process that affects the cerebral, coronary, and peripheral arterial circulation. There is some evidence that among patients with symptomatic atherothrombosis, 16% have symptomatic polyvascular disease. Thus, patients who have experienced an atherothrombosis-related ischemic event in one vascular territory are at risk for ischemic events in other vascular territories. This “cross risk” covers ischemic complications of ACS, cerebrovascular events (CVE)/ transient ischemic attacks, and peripheral arterial disease [6,7].
Stroke is a rare but feared complication of acute myocardial infarction. Hemorrhagic stroke within the first 24 hours is a wellknown consequence of thrombolytic therapy. However, in most cases, stroke following acute myocardial infarction is ischemic [8,9].
In patients with ST-segment elevation myocardial infarction (STEMI) treated with thrombolysis, the in-hospital incidence of hemorrhagic stroke is higher due to thrombolytic therapy. However, there has been more than 50% reduction of this incidence, recently, with the major contributor to this decrease being greater use of primary PCI at the expense of fibrinolytics.
However, it should be emphasized that the risk a hemorrhagic transformation in the case of an embolic stroke persists, due to anticoagulants and antiplatelet drugs’ use [4,10]. As observed in our patient, a primary PCI was performed instead of fibrinolytic treatment and he subsequently presented a cerebellar stroke with a hemorrhagic infarction under antiplatelet therapy. This observed outcome regarding the use of dual therapy corroborate those of the TRITON-TIMI (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction) trial, which suggest that dual antiplatelet therapy with aspirin and the novel thienopyridine, prasugrel, is associated with an increased risk of major bleeding, including intracranial hemorrhage, in patients with ACS and previous cerebrovascular events [11].
There is a detrimental correlation of stroke after ACS; the neurological deficit is greater, the clinical course more unfavorable, and mortality rates are higher compared to stroke patients free of ACS [3]. In our case study, this adverse correlation is confirmed by the existence of a significant cerebellar syndrome with worsening of the clinical condition and appearance of hemorrhagic infarction associated with cerebral edema that regressed after mannitol infusion.
Reports investigating lesion topography in the context of acute CVE in different subtypes of the TOAST classification, cerebellar infarcts have not been specifically analyzed [12,13], reflecting the lack of data in this category.
A number of studies examining patterns of infarction in the posterior cerebral circulation have found that cardioembolic etiologies were involved in 20-30% of cases [14,12]. Chung et al showed that 60% of superior cerebellar artery infarcts have an underlying cardioembolic source [12].
Data from the literature show that bilateral and multiple territory infarcts were more frequent in patients with a cardioembolic etiology than in patients without it, and that, in addition to the size of the infarct, the subsequent growth of the infarct and its hemorrhagic transformation were also strongly predictive of an underlying cardioembolic etiology, primarily AF [15,16,17].
Concerning our case, the ischemic brain injury was bilateral with the development of hemorrhagic infarction, most likely as a consequence of ACS, contrary to the studies suggesting AF as the cause of CVE [18]. We must point out that AF can’t be definitively excluded as a cause of the cerebellar stroke, in view of only a 24- hour Holter monitoring was carried out.
Conclusion
Acute coronary syndrome and stroke are both major causes of mortality. Their association is uncommon but it’s responsible of major increase in morbidity and mortality. Urgent and adequate management can sometimes improve the prognosis. We described a patient admitted for STEMI complicated 48 hours later with a bilateral cerebellar ischemic stroke associated with hemorrhagic infarction. This entity has been rarely described in the literature.
Conflict of Interest
None.
Funding
None received.
References
- Mendis S, Puska P, Norrving B (Eds.), (2011) Global atlas on cardiovascular disease prevention and control, vol. 3, World Health Organization, Geneva.
- Markle WH, Fisher MA, Smego RA Jr. (2007) Global health: past, present, and future Understanding global health (1st ed.), McGraw-Hill Professional pp. 11-12.
- Mooe T, Olofsson BO, Stegmayr B, Eriksson P (1999) Ischemic stroke. Impact of a recent myocardial infarction. Stroke 30(5): 997-1001.
- Brammås A, Jakobsson S, Ulvenstam A, Mooe T (2013) Mortality after ischemic stroke in patients with acute myocardial infarction: predictors and trends over time in Sweden. Stroke 44(11): 3050-3055.
- Kajermo U, Ulvenstam A, Modica A, Jernberg T, Mooe T (2014) Incidence, trends, and predictors of ischemic stroke 30 days after an acute myocardial infarction. Stroke 45(5): 1324-1330.
- Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, et al. (2006) REACH Registry Investigators. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 295(2): 180-189.
- Kannel WB (1994) Risk factors for atherosclerotic cardiovascular outcomes in different arterial territories. J Cardiovasc Risk 1(4): 333-339.
- Hess DC, D'Cruz IA, Adams RJ, Nichols FT 3rd (1993) Coronary artery disease, myocardial infarction, and brain embolism. Neurol Clin 11(2): 399-417.
- Gore JM, Granger CB, Simoons ML, Sloan MA, Weaver WD, et al. (1995) Stroke after thrombolysis. Mortality and functional outcomes in the GUSTO-I trial. Global Use of Strategies to Open Occluded Coronary Arteries. Circulation 92(10): 2811-2818.
- Tanne D, Gottlieb S, Hod H, Reicher-Reiss H, Boyko V, et al. (1997) Incidence and mortality from early stroke associated with acute myocardial infarction in the prethrombolytic and thrombolytic eras. Secondary Prevention Reinfarction Israeli Nifedipine Trial (SPRINT) and Israeli Thrombolytic Survey Groups. J Am Coll Cardiol 30(6): 1484-1490.
- Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, et al. (2007) TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357(20): 2001-2015.
- Chung JW, Park SH, Kim N, Kim WJ, Park JH, et al. (2014) Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification and vascular territory of ischemic stroke lesions diagnosed by diffusion-weighted imaging. J Am Heart Assoc 3(4): e001119.
- Bernstein RA, Di Lazzaro V, Rymer MM, Passman RS, Brachmann J, et al. (2015) Infarct Topography and Detection of Atrial Fibrillation in Cryptogenic Stroke: Results from CRYSTAL AF. Cerebrovasc Dis 40(1-2): 91-96.
- Amarenco P, Lévy C, Cohen A, Touboul PJ, Roullet E, et al. (1994) Causes and mechanisms of territorial and nonterritorial cerebellar infarcts in 115 consecutive patients. Stroke 25(1): 105-112.
- Rizos T, Bartsch AJ, Johnson TD, Dittgen F, Nichols TE, et al. (2017) Voxelwise distribution of acute ischemic stroke lesions in patients with newly diagnosed atrial fibrillation: Trigger of arrhythmia or only target of embolism? PLoS ONE 12(5): e0177474.
- Tu HT, Campbell BC, Christensen S, Desmond PM, De Silva DA, et al. (2015) EPITHET-DEFUSE Investigators. Worse stroke outcome in atrial fibrillation is explained by more severe hypoperfusion, infarct growth, and hemorrhagic transformation. Int J Stroke 10(4): 534-540.
- Jung JM, Kwon SU, Lee JH, Kang DW (2010) Difference in infarct volume and patterns between cardioembolism and internal carotid artery disease: focus on the degree of cardioembolic risk and carotid stenosis. Cerebrovasc Dis 29(5): 490-496.
- Kumral E, Kisabay A, Ataç C (2005) Lesion patterns and etiology of ischemia in superior cerebellar artery territory infarcts. Cerebrovasc Dis 19(5): 283-290.






























