Abstract
We aim to evaluate the effectiveness of endovascular thrombectomy performed within 24 hours in patients with ischemic stroke, comparing functional outcomes and mortality rates in relation to standard medical care. This is a systematic review not registered on the PROSPERO platform, with searches conducted in PubMed, SciELO, and LILACS databases. Randomized clinical trials involving adult patients were included. The findings indicate that endovascular thrombectomy, when performed early, improves functional recovery and reduces mortality, especially in cases of large vessel occlusion. Patients treated with thrombectomy showed better recanalization rates and higher quality of life. However, an increased risk of complications, such as intracranial hemorrhages, was observed in cases of larger infarcts. Endovascular thrombectomy is an effective intervention for improving clinical outcomes in patients with ischemic stroke, although greater care is needed in cases with more extensive infarcts.
Keywords: Ischemic stroke; Endovascular thrombectomy; Medical care
Abbreviations: LVO: Large Vessel Occlusions; MeVO: Medium Vessel Occlusions; IVT: Intravenous Thrombolysis; EVT: Endovascular Treatment; NCCT: Non-Contrast Computed Tomography
Introduction
According to Linhares et al. [1], ischemic stroke is a leading medical emergency globally, ranking as the second leading cause of death and the third leading cause of disability-adjusted life years lost. This type of stroke occurs due to the interruption of blood flow caused by a clot, leading to brain tissue damage and loss of neurological function. It accounts for approximately 80% to 85% of all strokes, highlighting its prevalence and severity. Immediate treatment is crucial to minimize brain damage and improve functional outcomes. In the management of acute ischemic stroke, recanalization therapies, including intravenous administration of thrombolytic drugs and endovascular thrombectomy, have proven effective in removing the blood clot and restoring cerebral blood flow, thereby reducing associated mortality and morbidity. According to Neto et al. [2], endovascular thrombectomy, in particular, has emerged as an innovative treatment for strokes caused by large vessel occlusion. This minimally invasive procedure involves inserting a catheter through an artery to the site of the clot, allowing for its mechanical removal. Furthermore, according to Roaldsen [3], the success of this intervention depends on several factors, including the careful selection of patients and the timely performance of the procedure. Studies indicate that patients with large cerebral vessel obstruction have a better prognosis when undergoing thrombectomy, especially if the treatment is performed within a specific time window after the onset of symptoms. Neto et al. [2] states that the decision to perform thrombectomy is based on the severity of symptoms, cerebral anatomy, the time elapsed since the onset of symptoms, and the patient’s overall clinical condition, aspects that are fundamental in determining who will benefit most from the procedure.
According to Cardoso et al. [4], the role of emergency medical services is essential in the initial management of patients with suspected stroke. Rapid identification of symptoms and urgent referral to specialized centers are critical for the success of treatment. Efficient protocols, such as the use of rapid assessment scales to detect large vessel occlusions and determine eligibility for reperfusion procedures, are essential to reduce the time between the onset of symptoms and therapeutic intervention. Neto et al. [2] emphasize that the NIHSS (National Institutes of Health Stroke Scale) is widely used to assess the severity of neurological symptoms and establish the severity of the clinical picture, thus assisting in the identification of the type of stroke and the most appropriate therapeutic decision. From Roaldsen’s perspective [5], recent studies have suggested that recanalization therapies, including endovascular thrombectomy, may be beneficial even for patients previously considered ineligible for thrombolytic treatment due to the unknown time of stroke onset. This advancement represents a paradigm shift in the approach to ischemic stroke, expanding the possibilities of treatment for a larger group of patients. However, the effectiveness of these interventions depends on an accurate assessment and an individualized approach, which considers not only the time window but also the complexity of the cerebral anatomy and the patient’s underlying health conditions. With the continuous evolution of imaging techniques and recanalization devices, it is expected that the effectiveness of endovascular thrombectomy will continue to improve, providing better functional outcomes and quality of life for patients affected by ischemic stroke. In this context, the present study aims to evaluate the effectiveness of endovascular thrombectomy performed within 24 hours after the onset of an ischemic stroke in improving patients’ functional outcomes, compared to standard medical care. To achieve this objective, specific comparisons will be made, such as comparing the rate of functional recovery between patients undergoing endovascular thrombectomy within 24 hours and those treated with standard medical care. In addition, it seeks to assess the difference in mortality rates between these two groups of patients, providing a more comprehensive understanding of the potential benefits of endovascular thrombectomy in acute ischemic stroke clinical scenarios.
Methods
TTS is an acquired condition most commonly affecting postmenopausal women who suffer a severe psychological or physical stressor. Concurring TTS and HCM presents mainly in females, with only half of them having being previously outlined with a known history of HCM. Although the approach to treat either condition separately is common practice, the simultaneous management of both entities in the acute phase poses a clinical challenge and relies on close monitoring and balancing of their opposing haemodynamic profiling.
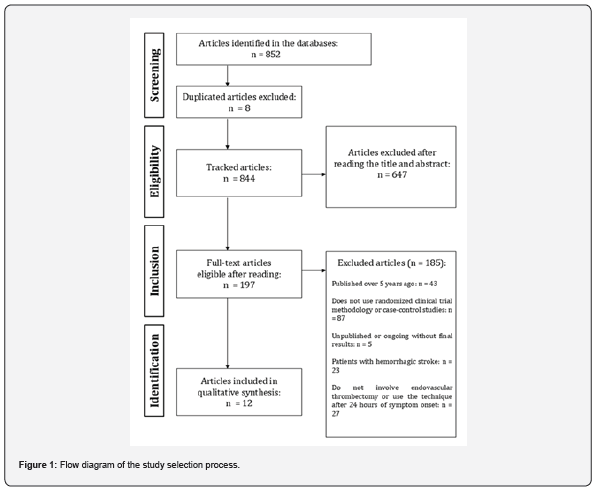
This systematic review study was not previously registered on the PROSPERO platform. The review stages, including screening, duplicate removal, and study selection, were performed using Zotero software. The conduct of this work followed the recommendations of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [4], ensuring transparency and standardization of all procedures.
Search Strategy
Three bibliographic databases were consulted: PubMed, SciELO, and the Latin American and Caribbean Literature on Health Sciences (LILACS). The search strategy included controlled descriptors: ((endovascular thrombectomy OR mechanical thrombectomy OR (endovascular therapy) OR (thrombectomy within 24 hours)) AND (ischemic stroke OR (acute ischemic stroke) OR (cerebral infarction)) AND (functional outcomes OR (clinical outcomes) OR (patient outcomes) OR (neurological function) OR (functional independence) OR (modified Rankin Scale) OR mRS OR (functional recovery)) AND (standard medical care OR (conservative treatment) OR (usual care) OR (standard therapy) OR (medical management)) AND (comparative study OR (comparison of outcomes) OR (difference in outcomes))). In addition, the keyword “Endovascular Thrombectomy” was used. The initial database search occurred in August 2024.
Eligibility Criteria
The inclusion criteria for this study encompass randomized clinical trials or case-control studies involving adult patients (≥ 18 years) with a confirmed diagnosis of ischemic stroke. These patients must have undergone endovascular thrombectomy within 24 hours of symptom onset and include those treated with standard medical care. Additionally, the studies considered must be published in English, Portuguese, or Spanish and have been published within the last five years. Conversely, the exclusion criteria include single case studies, review articles, commentaries, editorials, letters to the editor, unpublished studies, or ongoing articles without final results, as well as studies involving patients with hemorrhagic stroke or pediatric patients (under 18 years). Studies that do not specify the time between symptom onset and intervention, those that do not involve endovascular thrombectomy or use the technique after 24 hours from symptom onset, and studies that employ irrelevant or non-comparable outcomes will also be excluded.
Title and Abstract Assessment, Full-Text Reading, and Data Extraction
After importing the bibliographic references into Zotero software, the process of verifying and eliminating duplicates was initiated, both internally within each database and between the different databases used. Subsequently, two reviewers independently analyzed the titles and abstracts of the identified articles. The articles selected in this initial screening were subjected to full-text reading, also evaluated independently by two reviewers. In situations where differences of opinion occurred between the evaluators, a third reviewer was consulted to resolve the impasse. After the full-text reading of the studies, those that met all eligibility criteria were subjected to an assessment of methodological quality, followed by the extraction of relevant data. The narrative synthesis was developed from the collected information, including the year of publication, authors, article title, abstract, objectives, description of the methodology, main results, and conclusions.
Assessment of Methodological Quality
The methodological quality of the studies was assessed
independently by two researchers using the Cochrane tool for
randomized clinical trials (RoB 2). RoB 2 classifies the risk of bias
of the studies into three levels: “high,” “some concerns,” and “low,”
which increasingly indicate the susceptibility to biases that may
compromise the validity of the results obtained. This instrument
is applicable to various research designs and is composed of six
domains:
1) Randomization process,
2) Deviations from intended interventions,
3) Missing outcome data,
4) Measurement of the outcome,
5) Selection of the reported result, and
6) Overall assessment.
Methodological disagreements between the researchers’ evaluations were resolved by a third reviewer. No statistical analyses were performed.
Results
From 852 potentially relevant articles identified, where 8 were identified as duplicates and excluded, 197 publications were read in full, with 12 meeting the eligibility criteria and being included in the narrative synthesis. The flowchart of the study selection process is presented in Figure 1. The general characteristics of the selected studies are described in Table 1. The number of participants ranged from 36 to 780 individuals, involving patients with acute ischemic stroke, encompassing both large vessel occlusions (LVO) and medium vessel occlusions (MeVO). Most studies investigated the efficacy of mechanical thrombectomy, such as the study by Li et al. [6], which evaluated 318 patients with basilar artery occlusion treated between 6 and 24 hours after the onset of symptoms. Furthermore, the ESCAPE-MeVO study, led by Ospel et al. [7], included 530 patients to evaluate endovascular treatment in medium vessel occlusions. Regarding the type of study design, randomized clinical trials predominated. Silva et al. [8], for example, investigated mechanical thrombectomy with and without intravenous thrombolysis in 221 patients, while Premat et al. [9] analyzed the efficacy of intracranial stents in patients refractory to thrombectomy. The follow-up time ranged from 3 to 12 months, depending on the outcomes investigated, such as quality of life and recanalization rate, as highlighted in several studies (Table 1). Table 2 describes the results of the methodological quality assessment of the analyzed studies. According to the Cochrane tool (RoB 2), ten studies (83.33%) were classified as having a “low risk” of bias, while two (16.67%) had “some concerns” regarding bias. None of the studies were considered to have a “high risk” of bias. Based on the RoB 2 criteria, the main reasons for the “some concerns” classification in the studies were related to the measurement of outcomes. In some cases, the methodological assessment indicated weaknesses in the analyses of certain domains, such as the study by Ospel et al. [7], which, although assessed with a low risk in almost all aspects, had concerns regarding the measurement of outcomes. These methodological limitations may impact the interpretation of the outcomes, even though most of the studies maintained a robust methodological standard, with a low risk in various dimensions, such as the randomization process and the selection of reported outcomes.


Discussion
Endovascular Thrombectomy in Ischemic Stroke (Large Vessel Occlusion)
When comparing the studies by Li et al. [6] and Thomalla et al. [10], we observe complementary approaches that highlight the effectiveness of endovascular thrombectomy in different contexts of ischemic infarcts. Li et al.’s study [6], focusing on basilar artery occlusion, emphasizes the efficacy of thrombectomy in patients with basilar artery occlusion within a 6 to 24-hour window, underscoring the importance of intervention in cases of posterior stroke, which have high mortality and morbidity rates. In comparison, Thomalla et al. [10] addressed patients with established large infarcts, evaluating the long-term outcomes of thrombectomy in large vessel occlusions. The results indicate an improvement in the quality of life and survival of patients treated with thrombectomy, even in cases of extensive infarcts. Thus, the connection between the two studies lies in the evaluation of the effectiveness of thrombectomy in clinical contexts considered critical, whether due to the extent of the infarct or the location of the occlusion. In the study by Li et al. [6], the challenge is to treat patients with a high mortality rate, reinforcing that thrombectomy can improve recanalization and long-term functional outcomes. In the Thomalla et al. [10] study, the 12-month analysis demonstrates that, although the mortality rate remains high, thrombectomy offers functional and quality of life benefits for patients with larger infarcts. Both studies suggest that even in complex and high-risk scenarios, endovascular intervention can transform the prognosis of patients with stroke. Thus, it is possible to perceive that the findings reinforce the importance of long-term follow-up to understand the functional results. The second study highlights the benefits of thrombectomy, showing that early interventions improve the quality of life in stroke patients, complementing the first by carefully evaluating risks and benefits.
Furthermore, when comparing the studies by Silva et al. [8], Premat et al. [9], and Marko et al. [11], focused on thrombectomy and its variations, we observe how different approaches to the treatment of ischemic stroke with large vessel occlusions offer complementary perspectives. The study by Marko et al. [11] showed that, despite the complexity of tandem carotid occlusions, the long-term results were comparable to those of patients without these lesions. The decision to perform cervical stenting did not affect functional outcomes, suggesting that thrombectomy already brings substantial benefits. Moreover, this perspective is complemented by the study by Premat et al. [9], which focuses on occlusions refractory to conventional thrombectomy treatment. Where rescue intracranial stenting is a promising option after thrombectomy failure, increasing recanalization, but with an elevated risk of hemorrhagic complications due to antithrombotic therapy. When compared to Marko et al. [11], where cervical carotid stenting did not decisively influence functional outcomes, the study by Premat et al. [9] presented a more aggressive approach, suggesting that intracranial stenting may be essential in cases of refractory occlusion, but with a higher risk.
Also, it is possible to note that the study by Silva et al. [8] offers an analysis of intravenous thrombolysis (IVT) before thrombectomy, concluding that the combination of IVT with thrombectomy did not improve functional outcomes when compared with thrombectomy alone. This evidence suggests that, in certain contexts, direct thrombectomy may simplify treatment without compromising results. Thus, by connecting these three studies, we observe a common thread: the treatment of complex or refractory occlusions, whether with or without the addition of IVT or stents, can be optimized if the assessment of hemorrhagic risks and successful recanalization are considered, highlighting the importance of personalized interventions for each clinical profile. Interventions with Thrombectomy and Additional Therapies In the comparison between the studies of adjunct thrombolysis [11] and direct thrombectomy [12], we find a complementary approach on the effectiveness of different strategies to optimize the treatment of ischemic stroke, highlighting the complexity of therapeutic decisions. The study on the use of intra-arterial alteplase post-thrombectomy demonstrates that even after successful recanalization, there is still a risk of microvascular hypoperfusion, which compromises the long-term clinical outcome. The administration of alteplase after thrombectomy aims to dissolve microthrombi that are not resolved by mechanical intervention, providing more effective cerebral reperfusion and improving neuronal and functional recovery. This finding highlights the importance of addressing not only angiographic success but also the quality of reperfusion in the capillaries, a dimension that, although subtle, can be decisive for the prognosis.
In contrast, the study by Mitchell et al. [13] seeks to evaluate the feasibility of direct thrombectomy, without the prior use of intravenous thrombolysis, a practice that could simplify treatment and minimize risks such as intracerebral hemorrhage, frequently associated with the use of alteplase. This approach, although showing results comparable to bridging therapy in terms of functional outcomes, raises questions about the need to further optimize the management of patients who, in theory, could benefit from both thrombectomy and intravenous thrombolysis. Thus, in a broader discussion, both studies complement each other by demonstrating that the central issue in the treatment of ischemic stroke is not only the recanalization of the main vessel but the quality of the subsequent reperfusion. While the study with post-thrombectomy alteplase addresses a potential solution to improve cerebral microcirculation, the second study questions whether simplifying the process with direct thrombectomy can offer similar benefits with less risk. Thus, the combination of these two perspectives suggests that future strategies may benefit from a hybrid approach, considering both the safety and efficiency aspects of cerebral reperfusion.
Medium Vessel Occlusion and Therapeutic Alternatives
When comparing the articles by Ospel et al. [7] and Nguyen et al. [14] on endovascular treatments for cerebral vessel occlusion, some similarities and differences emerge, revealing important nuances in the application and results of these treatments. The study by Ospel et al. [7] focuses on medium vessel occlusions, suggesting that endovascular treatment (EVT) may improve outcomes compared to traditional medical management for patients suffering from ischemic stroke (stroke). On the other hand, Nguyen et al. [14] focuses on large vessel occlusions (LVO) presented in a late window (6 to 24 hours), using non-contrast computed tomography (NCCT) to select patients for EVT. Both studies seek to improve the neurological outcomes of stroke patients, but Ospel et al. [7] points to a smaller margin of benefit due to the greater complexity and risk associated with smaller vessel occlusions. Thus, it is possible to perceive that while the article on EVT in LVO emphasizes the effectiveness of thrombectomy even outside the traditional treatment window, the first article raises the uncertainty regarding the risks of the procedure in smaller vessels. NCCT, as a selection tool, proves effective in identifying candidates in an expanded window scenario, an advance that complements the more conservative approach of ESCAPE-MeVO. This demonstrates a difference in time and risk management between the two types of occlusions, with EVT being potentially more beneficial for LVO in a late window, while for MeVO, the decision to apply EVT should be more carefully considered due to the additional risks. Thus, the two studies complement each other by providing insights on how to optimize EVT based on the type and timing of the occlusion, helping to shape the future of clinical decisions in stroke management.
Quality of Life and Functional Outcomes
When analyzing the studies on endovascular treatment for ischemic stroke, we can observe complementary approaches and comparisons that illustrate the development and challenges of this intervention in different contexts. The study by Joundi et al. [15] investigated the health-related quality of life after endovascular thrombectomy, showing an improvement in quality of life at 90 days, especially in older patients. Thrombectomy reduced functional disability, with a positive impact on various dimensions of physical and social well-being. The study highlights the importance of evaluating not only survival but quality of life as an essential outcome in the treatment of ischemic stroke. On the other hand, it is noted that the study by Lansberg et al. [16] focused on the effectiveness of thrombectomy performed in a window of 6 to 16 hours after the stroke. It showed that thrombectomy benefits various patients, regardless of age or location of the occlusion, suggesting improvement in functional outcomes, even with intervention in extended times. In comparison with the study by Joundi et al. [15], which prioritized quality of life, Lansberg et al. [16] focused more on functionality and survival, revealing that thrombectomy is effective even in more complex and later situations.
However, compared to the other two studies, Huo et al. [17] addressed thrombectomy in patients with large cerebral infarcts, a population generally excluded from previous studies. The results indicate that thrombectomy can be beneficial but presents an elevated risk of intracranial hemorrhages. This introduces an important nuance when comparing with the two previous studies, which showed consistent benefits with less hemorrhagic risk. Huo et al. [17] suggests that, although thrombectomy can be extended to patients with large infarcts, the increased risk of complications requires careful assessment to balance the benefits and risks. Together, these three studies offer a comprehensive view on endovascular thrombectomy, from the improvement of quality of life and functionality in different age groups to the possibility of expanding the use of the treatment for more severe cases. They demonstrate that, although thrombectomy is effective, its application in patients with large cerebral infarcts requires a more cautious approach due to the increased risk of hemorrhagic complications [18]. Thus, these studies complement each other by highlighting the advances and limitations in the adoption of thrombectomy as the treatment of choice for ischemic stroke.
Conclusion
The present systematic review has demonstrated that endovascular thrombectomy, when performed within 24 hours of the onset of ischemic stroke symptoms, is effective in improving patients’ functional outcomes compared to standard medical care. The reviewed studies indicate that, in patients with large vessel occlusion, early intervention can reduce mortality and increase quality of life. Despite the variability in outcomes across the studies, the majority point to a clear advantage of thrombectomy, especially in terms of recanalization and functional recovery, provided it is performed within the recommended time window. However, there are still limitations regarding the application of thrombectomy in cases of larger infarcts and the risk of hemorrhage in specific profiles. Careful patient selection is essential, and the quality of cerebral reperfusion, as well as the need for complementary interventions such as intra-arterial thrombolysis, require further studies and in-depth investigations.
References
- Linhares MR, Oliveira GML de, Jaculi AJD, Freire NVHM, Moura GM, et al. (2024) A utilização de trombectomia mecânica no tratamento do Acidente Vascular Cerebral isquêmico agudo: uma revisão de literatura. STUDIES IN HEALTH SCIENCES 5: e3983.
- De Oliveira Neto N, Campos GF, Alves LM, Fonsec, TMA, Santos KN, et al. (2023) Avc: Avaliação Clínica E Necessidade De Trombectomia. Revista Foco 16(9): e2978.
- Roaldsen MB, Lindekleiv H, Mathiesen EB. Intravenous thrombolytic treatment and endovascular thrombectomy for ischaemic wake-up stroke. Cochrane Database of Systematic Reviews. 2021.
- CARDOSO (2024) Jean Matheus Guedes et al. Principais estratégias de manejo no tratamento do AVC (isquêmico e hemorrágico). Journal of Social Issues and Health Sciences (JSIHS), [S. l.] 1(4).
- B Roaldsen M, Lindekleiv H, B Mathiesen E (2024) Tratamento trombolítico intravenoso e trombectomia endovascular para acidente vascular cerebral isquêmico:: uma revisão Cochrane. JBMEDE - Jornal Brasileiro De Medicina De Emergência 3(4).
- Li C, Wu C, Wu L, Zhao W, Chen J, et al. (2022) Basilar Artery Occlusion Chinese Endovascular Trial: Protocol for a prospective randomized controlled study. Int J Stroke 17(6): 694-697.
- Ospel JM, Dowlatshahi D, Demchuk A, Volders D, Möhlenbruch M, et al. (2024) Endovascular treatment to improve outcomes for medium vessel occlusions: The ESCAPE-MeVO trial. Int J Stroke 19(9): 1064-1070.
- Silva GS, Alves MM, Barros FCD, Frudit ME, Pontes-Neto OM, et al. (2024) The role of intravenous thrombolysis before mechanical Thrombectomy: A subgroup analysis of the RESILIENT trial. J Neurol Sci 457: 122853.
- Premat K, Dechartres A, Baptiste A, Guedon A, Mazighi M, et al. (2025) Comparison of rescue intracranial stenting versus best medical treatment alone in acute refractory large vessel occlusion: study protocol for the PISTAR multicenter randomized trial. J Neurointerv Surg 17(4): 360-367.
- Thomalla G, Fiehler J, Subtil F, Bonekamp S, Aamodt AH, et al. (2024) Endovascular thrombectomy for acute ischaemic stroke with established large infarct (TENSION): 12-month outcomes of a multicentre, open-label, randomised trial. The Lancet Neurology. 23: 883-892.
- Marko M, Cimflova P, Poppe AY, Kashani N, Singh N, et al. (2022) ESCAPE-NA1 investigators. Management and outcome of patients with acute ischemic stroke and tandem carotid occlusion in the ESCAPE-NA1 trial. J Neurointerv Surg 14(5): neurintsurg-2021-017474.
- Laredo C, Rodríguez A, Oleaga L, Hernández-Pérez M, Renú A, et al. (2022) Adjunct Thrombolysis Enhances Brain Reperfusion following Successful Thrombectomy. Ann Neurol 92(5): 860-870.
- Mitchell PJ, Yan B, Churilov L, Dowling RJ, Bush S, et al. (2022) DIRECT-SAFE: A Randomized Controlled Trial of DIRECT Endovascular Clot Retrieval versus Standard Bridging Therapy. J Stroke 24(1): 57-64.
- Nguyen TN, Nogueira RG, Qureshi MM, Nagel S, Raymond J, et al. (2024) Noncontrast CT Selected Thrombectomy vs Medical Management for Late-Window Anterior Large Vessel Occlusion. Neurology 102(10): e209324.
- Joundi RA, Rebchuk AD, Field TS, Smith EE, Goyal M (2021) Health-Related Quality of Life Among Patients With Acute Ischemic Stroke and Large Vessel Occlusion in the ESCAPE Trial. Stroke 52(5): 1636-1642.
- Lansberg MG, Mlynash M, Hamilton S, Yeatts SD, Christensen S, et al. (2019) Association of Thrombectomy with Stroke Outcomes Among Patient Subgroups: Secondary Analyses of the DEFUSE 3 Randomized Clinical Trial. JAMA Neurol 76(4): 447-453.
- Huo X, Ma G, Tong X, Zhang X, Pan Y, et al. (2023) Trial of Endovascular Therapy for Acute Ischemic Stroke with Large Infarct. N Engl J Med 388(14): 1272-1283.
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7): e1000097.






























